Introduction
Treatments done in pediatric dentistry not only have an immediate effect on pain felt by the child, but also has long term effects on the functionality, esthetics, and stability of occlusion. Hence, any decision regarding dental treatment in a child, should also take long term consequences into consideration to prevent iatrogenic orthodontic treatments in the future.
Case Report
A 13 year old male child reported to the clinic with a complaint of pain in lower right back region of teeth since 15 days, with bleeding from the same tooth for the past one week.
Patient was completely asymptomatic 15 days back and then he noticed pain in his lower right back region of teeth. Pain was sharp and persistent, which aggravated on taking hot and cold foods, and persisted even after removal of the stimulus. Pain subsided after taking medication.
On extra oral examination, no abnormality was detected in hairline, skin, eyes, nose, ears, lips, nails, lymph nodes and TMJ.
On intra oral examination, a grossly carious lesion was seen in 46. Generalised stains and calculus was seen. The dentition was entirely permanent dentition, with a Class I molar and canine relationship. The overjet was 3 mm and overbite was 4 mm. No abnormality was detected on soft tissue examination.

(This is a case report for space maintenance in a permanent dentition. To read a case report on space maintenance in a primary dentition, you may click here.)
Hard Tissue Examination
- Teeth present- (Permanent dentition)
- 17, 16, 15, 14, 13, 12, 11, 21, 22, 23, 24, 25, 26, 27, 37, 36, 35, 34, 33, 32, 31, 41, 42, 43, 44, 45, 46, 47
- Stains/Calculus – +/++
- Grossly carious IRT 46
- Molar relationship- Angle’s class I
- Canine relationship- class I
- Overjet – 3 mm
- Overbite – 4 mm
Provisional diagnosis was chronic irreversible pulpitis in 46. An intraoral periapical radiograph was taken and the final diagnosis was confirmed to be a chronic alveolar abscess.

Treatment Plan
- Emergency Phase: Not required
- Medical/Systemic Phase: Not required
- Preventive Phase: Oral hygiene instructions given
For the preparatory phase, oral prophylaxis, followed by fluoride application was done. Oral hygiene instructions were given.
For the corrective phase, extraction of 46 followed by prosthetic rehabilitation was planned, with a periodic recall and follow up every 3 months.
- Maintainence Phase: Periodic recall and follow up every 3 months.
Corrective Phase

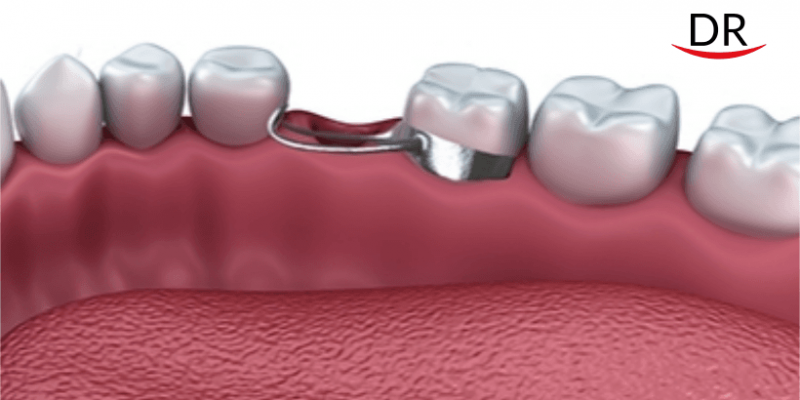
After extraction of 46, banding was done IRT 45 and 47 and then an impression was made. The band was transferred to the impression and stabilised. Cast was then poured using dental stone and and a meshwork of thin wire was made between the two teeth. After that with help of wax, the teeth was stabilised in the meshwork onto the cast. Then try in was done in the oral cavity. Occlusion was checked and find cementation was done using luting GIC.

Discussion
Ideally, as the occlusion develops from the primary dentition through the transitional (or mixed) dentition to the permanent dentition, a sequence of events occurs in an orderly and timely fashion. These events result in a functional, aesthetic, and stable occlusion.
When this sequence is disrupted, however, problems arise that may affect the ultimate occlusal status of the permanent dentition. When such disruptions do occur, appropriate corrective measures are needed to restore the normal process of occlusal development. Such corrective procedures may involve some type of passive space maintenance, active tooth guidance, or a combination of both.
In this case, the bridge provides us with an additional treatment modality in case of an early loss of a permanent tooth in young adolescent patients. It has soft tissue sparing as compared to a treatment partial denture. Success of bonded prosthesis is variable, design-dependent and requires the abutment teeth to have adequate structure and sound enamel for etching and bonding.
The bridge is functional, readily acceptable, maintains the mesiodistal dimensions of the lost tooth, prevents supra eruption of opposing teeth and does not restrict normal growth and development, as is required of an ideal space maintainer.
Conclusion
The permanent first molars are of utmost importance and all the measures should be tried to preserve them in the oral cavity. In case of loss of the structure or tooth, it is important to restore them for proper functioning and maintenance of occlusion. Restoring them endodontically and/or prosthetic rehabilitation should be considered in case of severe loss of tooth structure or the entire tooth.
References
- Horax H. Management of premature loss of primary first molar case with simple fixed space maintainer. Dentofasial. 2009; 8(1): 23- 26
- Goenka P, Sarawgi A, Marwah N, Gumber P, Dutta S, Simple Fixed Functional Space Maintainer. Int J Clin Pediatr Dent 2014; 7(3):225-228
- Aquilino S A, Caplan D J. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002; 87:256–63















Comments