PRP Platelet Rich Plasma in Dentistry
BLOOD DERIVATIVES: PRP Platelet Rich Plasma in Dentistry
- PRP Platelet Rich Plasma in Dentistry (PRP)
- Platelet Rich Fibrin (PRF)
- Advanced Platelet Rich Fibrin (A-PRF)
- Injectable Platelet Rich Fibrin (I-PRF)
Introduction: PRP Platelet Rich Plasma in Dentistry
PLATELET RICH PLASMA (PRP): PRP Platelet Rich Plasma in Dentistry
The regenerative growth factor found in platelets, which are the reparative EQUIPMENTS: the procedure should involve the use of all sterile instruments.
- Disposable Syringe To Collect Patients Blood
- Sterile Gauze Piece Or Swab
- Blood Collection Tubes
- Centrifugal Machine
PRP is an advanced treatment which has played a key role in wound healing and soft tissue regeneration, a well-known technique in maxillofacial procedures, sports medicine and cardiovascular surgery,
PRP is a minimally invasive procedure and now used with great success for aesthetic purposes due to cells in our body.
USES
- PRF when used in conjunction with bone grafts can offer several advantages including promoting wound healing, bone growth and maturation, graft stabilisation, wound sealing and homeostasis and improving the handling properties of graft material.
- PRF can also be used as a membrane.
- PRF can also be used to treat gingival recession.
INJECTABLE-PRF (I-PRF)
PRP has found its uses in regenerative dentistry as a supra-physiological concentrate of autologous growth factors, which is capable of stimulating tissue regeneration.
Despite this, many scientific papers have expressed concerns regarding the use of anti-coagulants, agents which are known to inhibit wound healing. In one study, a liquid formulation of injectable platelet rich fibrin (I-PRF) without the use of anti-coagulants was investigated.
This “super PRF” is produced with new type of tubes I-PRF specifically indicated for this preparation. The use of I-PRF in dentistry is in its early stages, but already the results in both oral surgery and regenerative medicine are very promising. Injection into the soft tissues usually increases vascularity and which will perhaps improve the biotype, injection into the bone graft particles (biomaterials) in order to coagulate and get a ‘solid’ which will be free of all movement granules. The graft clot interests lies in how to carve a bone graft and give it a compact form.
The protocol for I-PRF is a real scientific and clinical innovation and will allow many dental surgeons to improve their results in bone grafts.
Standard PRP and I-PRF (centrifuged at 700 rpm (60G) for 3min) were compared for growth factor release up to 10 days (8 donor samples). Furthermore, fibroblast biocompatibility at 24 h (live/dead assay); migration at 24h; proliferation at 1, 3, and 5 days, and expression of PDGF, TGF-S, and collagen1 at 3 and 7 days were investigated.
Advanced Platelet Rich Fibrin (A-PRF) is a new advanced form of PRF that can help heal wounds anywhere in the body and also those sites involved in oral surgery, using the patient’s own blood . Unlike in Platelet Rich Plasma (PRP), A-PRF doesn’t contain additives. In addition to that, A- PRF is very rich in platelets, leukocyte cells (growth factor cells) and contains enriching fibrin – the most key ingredient responsible for initiating the healing of wound, with added antibacterial properties.
A-PRF is more advanced than PRP due to having 20 times more leukocytes cells. It can be used inside of extraction sockets and around the dental implants to fast-track the process of bone and gum formation. It allows the implant to heal at an accelerated rate.
When a wound is detected in the body, the healing process is initiated by rushing different cells to the wound. One of the main cell types is platelets. Platelets circulating in our blood are the cells which bind together when they recognize damaged blood vessels.
When you get a cut or a wound, the platelets bind together at the site causing a blood clot which stops us from bleeding. This stimulates stem cells that help create new tissues. This overall process allows the body to heal faster and more efficiently.
CLINICAL APPLICATIONS OF PRP Platelet Rich Plasma in Dentistry
PRP Platelet Rich Plasma in Dentistry
BONE REGENERATION
- Sinus lift grafting
- Ridge augmentation
- Repair of bone defects created by removal of teeth or small cyst
- Ridge preservation techniques
- Periodontal defects
- Closure of cleft lip and palate defects
- Repair of oro-antral fistulas
- Craniofacial reconstruction
SOFT TISSUE REGENERATION
- Periosteal and connective tissue flaps
- Free connective tissue and gingival grafts
- Root coverage procedures
- Controling soft tissue healing and tissue maturity
- NON DENTAL
- Acne Scars Removal
- Hair Growth
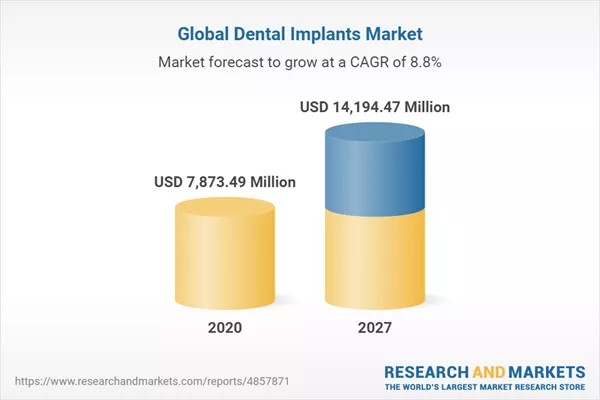
PRP WITH IMPLANTS
Fontana et al. found a higher amount of peri-implant bone volume after inserting PRP and laminar test implants into rat tibial sites. Fuerst et al.
Defined platelet rich in growth factors (PRGF), as the supernatant from washed; thrombin-activated, allogenic, platelet-rich plasma obtained after centrifugation and used this solution with implants with success to increase in BIC.
Few studies also advocated the benefits of topical application with implants before insertion, and saw effects in early healing. On the other hand, Weibrich et al. failed to see any benefit on BIC from PRP in their trial in rabbits. In a recent study titanium non-coated AIO grit-blasted and acid etched,and 18 magnetron-sputtered calcium phosphate (CaP) coated titanium ( femoral condyles in six goats. PRP was used as a test modality, as some implants were dipped in PRP before insertion and other implants were placed into sites where PRP-gel had been previously inserted.
Results and conclusions were that CaP coated implants rendered higher values for BIC than the rough implants used as control. No additive value for PRP was found except at an early healing stage.
PERI-IMPLANT DEFECTS AND PRP
A general extensive literature overview on marginal defects around implants has been presented by Boticelli (2006), Yamada et al. found similar results of tissue engineered bone and autologous bone after grafting and installation of implants in two stages. BIC values for implants were comparable between the sides in that study. Kim et al.used freeze-dried bone and dentin-like material as filler material with and without PRP and found better results with respect to BIC with the addition of PRP.
Sanchez et al. failed to see more than a low effect of PRP combined with demineralized freeze-dried bone in 3-walls defects in the mandible of dogs. In another study by Casati et al. a buccal dehiscence implant defect model was used in dogs and the defects were randomly filled with PRP or blood as control. No effects on regeneration of that type of defect could be seen.
Conclusion: PRP Platelet Rich Plasma in Dentistry
PRP therapy has evolved a long way from just use in Dermal / Cosmetology procedures to innovative uses in Dentistry. While lot of Studies, Research is underway uses & efficacy of PRP is expected to increase manifolds in the field of Dentistry.















Great blog post.Helpful and informative tips. I like it thanks for sharing this information with us