Platelet concentrate is nothing but a centrifuged blood with only platelets and fibrin in maximum amount and less or very few leucocytes at the bottom. Other components get separated from the platelet concentrates in the upper layer. Several techniques for platelet concentrates are available. This is because of the commercialization and also their applications have been confusing, each method leads to a different product with different biology and potential uses. Development of bioactive surgical additives regulating inflammation with increasing healing is a great challenge and even after each intervention, surgeons face complex tissue remodeling phenomena affecting healing and tissue survival. To limit such consequences autologous grafting and regeneration have been researched.
Platelet concentrates are classified on their leucocyte, fibrin content and method of preparation.
- Pure Platelet-Rich Plasma (P-PRP), such as cell separator PKP, vivostat PRF or Anitua’s PRGF.
- Leucocyte-and Platelet-Rich Plasma (L-PRP), such as Curasan, Kegen, Plateltex, Smart PReP, PCCS, Magellan or GPS PRP.
- Pure Platelet Rich Fibrin (PRGF), such as Fibrinet and Leucocyte.
- Platelet-Rich Fibrin (L-PRF), such as Choukroun’s PRF, T-PRF (Titanium PRF), I-PRF (Injectable PRF), A-PRF (Advance PRF) all these variants are due to either differences between centrifuge speed or use of titanium as a collection tube instead of normal glass tubes or vacuum blood collection tubes.
- Concentrated Growth Factors (CGF).
Why platelets concentrate is so popular?
Platelets concentrate is popular because they contain growth factors essential for regeneration and early wound healing.
Growth factors present in platelets
| Growth Factors | Primary functions |
| Epidermal growth factors (EGP) | Regulation of cell proliferation, differentiation, and survival. |
| Insulin like growth factors IGF | Key regulators of cell metabolism and growth
Stimulates proliferation and differentiation functions in osteoblast |
| Platelet derived growth factor | Mitogen for connective tissue cells and other cell types. Enhance the synthesis of collagen and structural proteins |
| Transforming growth factors alpha beta | Regulation of cell proliferation, differentiation and apoptosis
Induction of intimal thickening |
| Vascular endothelial growth factor | Regulation of angiogenesis |
- Epidermal Growth factors (EGP)
- Regulation of cell proliferation, differentiation and survival.
- Insulin like growth factors IGF
Key regulators of cell metabolism and growth
Stimulates proliferation and differentiation functions in osteoblast. Mitogen for connective tissue cells and other cell types enhance the synthesis of collagen and structural proteins.
Regulation of angiogenesis and method of preparation of PRP:
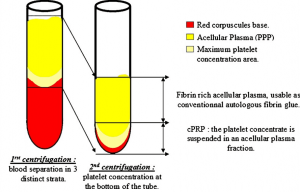
- Venous blood is drawn and mixed with anticoagulant to avoid platelet activation and degranulation.
- The first soft spin centrifugation separates blood in 3 distinct layers:
- The red blood corpuscles constitute 55% of total volume form the bottom layer of the tube.
- The acellular plasma layer is mainly made up of fibrinogen and low in platelets called as Platelet-Poor Plasma (PPP) and constitutes 40% of total volume forms a top layer of the tube.
- Between the 2, an intermediate layer is where platelets concentrations are largely increased. It constitutes only 5% of total volume called as buffy coat. It will compose the major part of the future PRP, but at this stage, it is non separable completely.
- A sterile syringe is used to aspirate PPP, PRP and some red blood corpuscles, the remaining content is transferred to another tube which is anticoagulant less.
- This second tube will then undergo another centrifugation, purported to be longer and faster than the first (‘‘hard spin’’). This makes it possible to concentrate platelets at the bottom of the tube and subsequently to obtain once again 3 distinct layers some residual red blood corpuscles trapped at the bottom of the tube and at the top acellular plasma (PPP) consists of 80% of total volume and between these two a buffy layer called PRP.
- It becomes easy to collect the PRP at this stage. Major part of the PPP is discarded by using a syringe, just leaving some serum to place the platelet concentrate in suspension. The unit is then gently shaken to obtain a ready-to-use PRP. Note that the red blood corpuscles trapped at the bottom of the tube are also suspended by this last operation, which explains the rosy aspect of the final PRP.
- PRP is then mixed with bovine thrombin and calcium chloride at the time of application, with the help of a mixing syringe. Gelling of platelet concentrate will then quickly occur: Fibrinogen is also concentrated during the PRP preparation and its polymerisation will constitute a fibrin matrix with particularly interesting homeostatic and adhesive properties.
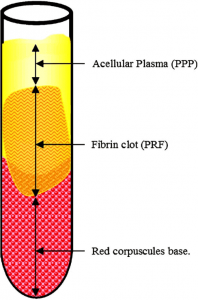
PRF preparation
PRF protocol is very simple compared to PRP. Venous blood is drawn without anticoagulant in 10 ml tubes which centrifuged immediately at 3000 rpm (approximately 400 g) for 10 minutes. Care in handling of blood and quick action is required.
Properties of PRF
- Contains intimate assembly of cytokines, glycanic chains, structural glycoproteins enmeshed between slowly polymerized fibrin network
- Considered as an immune node which stimulates defense mechanism
- Significant inflammatory response at surgical site after PRF placement due to cytokines enmeshed within the matrix
Application in Periodontics
- Treatment of Intrabony Defects – PRP alone or in combination with bone grafts, PRF alone or in combination with bone grafts have shown adequate regeneration than only open flap debridement
- Treatment of furcations involvement – PRP alone or in combination with bone grafts, PRF alone or in combination with bone grafts have shown bone regeneration in class 2 class 3 furcation cases
- Ridge augmentations
- Sinus perforation repair by using PRF membrane
- Gingival recession treatments
- Papilla reconstruction using PRF
- Socket preservation after extraction
- Enhance the healing at palatal wound after Free Gingival Graft.
Advantages of PRF over PRP
- No bovine thrombin or anticoagulant is used
- Single centrifuge cycle requires
- Easy handling
- Even act as a vehicle for tissue engineering
Conclusion:
PRPs are often considered as improved fibrin glues without consistency, however PRFs can be regarded as dense fibrin biomaterial with biomechanical properties. A dese fibrin clot can serve as a biological healing matrix. It supports cell migration and cytokine release. Expensive and complex procedures cannot always used in daily practice and many will disappear with time. Simple and free systems such as Choukroun’s PRF were developed by clinicians for clinicians and are anticipated to be major methods in the coming years. PRF have many advantages and prepared by chair side with less time, no complicated method of preparation, simple handling makes it a better choice in periodontal procedures.
References
- Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): A second-generation platelet concen-trate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:e37-e44.
- Dohan DM , Rasmusson L and Albrektsson T Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte and platelet-rich fibrin(L-PRF). Trends in Biotechnology Vol.27 No.3
Bonus: Download our monthly e-bulletin! Click here to get it
DISCLAIMER : “Views expressed above are the author’s own.”

















Comments