Diabetes is the most common disease in India and every year the number of people diagnosed with diabetes is ever increasing, current data shows more than 62 million people suffer with the disease. India tops the list for maximum individuals diagnosed with diabetes mellitus (31.7 million) followed by China (20.8 million) and United States (17.7 million) according to 2000 statistics. Diabetes mellitus is metabolic disorder characterized by high glucose level in blood. It a syndrome of abnormal carbohydrate, lipid and protein metabolism that results in acute and chronic complications due to the absolute or relative lack of insulin. There are three types of diabetes: Type 1, which results from an absolute insulin deficiency; Type 2, which is the result of insulin resistance and an insulin secretory defect; and gestational, a condition of abnormal glucose level during pregnancy. Keeping in mind the increasing prevalence of diabetes in the world’s population day by day International Diabetic Federation and WHO created World Diabetic Day (WDD) to spread diabetes awareness. WDD was decided as 14 November after the birthday of Sir Frederick Banting, the co-discoverer of insulin along with Charles Best in 1922. WDD has become the world’s largest diabetes awareness program which is reaching a global population in more than 160 countries. This campaign highlights the importance of awareness about diabetes in the global population.
The WDD campaign aims to
- Be the platform to promote IDF advocacy efforts throughout the year.
- Be the global driver to promote the importance of taking coordinated and concerted actions to confront diabetes as a critical global health issue.
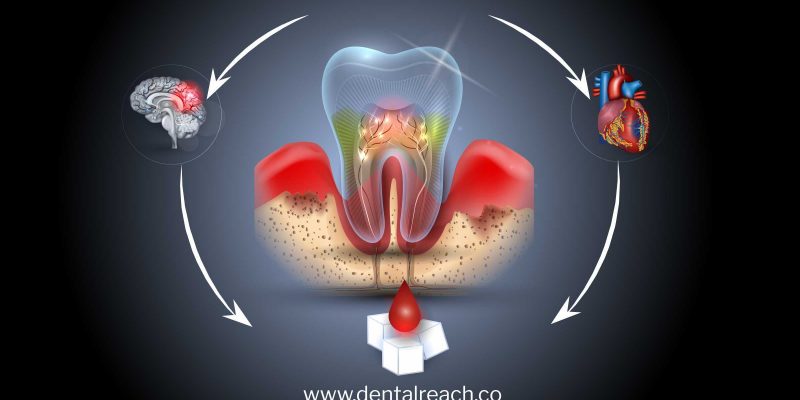
Diabetes is a multifactorial disease. The causative factors includes genetic factors coupled with environmental influences such as obesity associated with rising living standards, steady urban migration and lifestyle changes. Lack of exercise, no fixed timings for meals or skipped meals because of a busy lifestyle resulting in abnormal metabolism and some of the causative factor for developing diabetes mellitus. Diabetes mellitus impairs many other systems of the body and develops different diseases in the body and hence many diseases and symptoms are often correlated with the diabetes mellitus. There is also a correlation between oral health and the diabetes.
Classification of diabetes
Type 1 diabetes (formerly insulin-dependent diabetes)
Type 2 diabetes (formerly non-insulin-dependent gestational diabetes, other types of diabetes)
- Genetic defects in p cell function
- Genetic defects in insulin action
- Pancreatic diseases or injuries
Pancreatitis, neoplasia, cystic fibrosis, trauma, pancreatectomy
- Infections
Cytomegalovirus, congenital rubella
- Drug-induced or chemical-induced diabetes
Glucocorticoids, thyroid hormone
- Endocrinopathies
Acromegaly, pheochromocytoma, glucagonoma, hyperthyroidism, Cushing’s syndrome
- Other genetic syndromes with associated diabetes
Signs and symptoms of diabetes
Polyuria, polydipsia, polyphagia these are the classical triad associated with diabetes mellitus. Along with this, weight loss, irritability, fatigue and mental confusion also common findings. In long standing, poorly controlled hyperglycemia cases, microvascular and macrovascular conditions may develop that can produce retinopathy, cataracts, nephropathy, neuropathy and paresthesia and atherosclerosis as well as recurrent infections and impaired wound healing. Oral malodor like fruity breath presents with acute hyperglycemia cases.
Diagnosis
Lab diagnosis
Random casual non fasting glucose level ≥ 200 mg/dl
Fasting plasma glucose level ≥ 126 mg/dl
Post prandial plasma glucose level ≥ 200 mg/dl
HbA1c test is used to measure effectivity of diabetic drugs.
Oral manifestations of the diabetes
- Burning mouth syndrome
- Candidiasis – a fungal infection
- Dental caries
- Gingivitis
- Glossodynia
- Lichen planus
- Neurosensory Dysesthesias
- Periodontitis
- Salivary dysfunction
- Xerostomia
Gingivitis and periodontitis
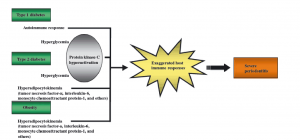
There is also an association between periodontitis and diabetes mellitus and it is considered as two way mechanism that means diabetes can cause periodontitis as well as severe periodontitis can results in to diabetes mellitus. In diabetic patients there is altered host defense, altered subgingival microflora, alter collagen synthesis and metabolism, defects in PMNs (polymorphonuclear leukocytes), Increased AGE (advanced glycosylation end products) formation. Multiple pathophysiological mechanisms (compromised neutrophil function, decreased phagocytosis and leukotaxis) also responsible for the increased alveolar bone loss in diabetic patients. Multiple periodontal abscesses is a common finding in uncontrolled diabetic patients.
Dental caries
In diabetic patients there is abnormal salivary function leading to dry mouth, periodontal diseases and abnormal oral sensory functions which could increase their risk of developing new and recurrent dental caries.
Salivary dysfunction
People with diabetes often complain of dry mouth or xerostomia and experience salivary gland dysfunction. Impaired salivary uptake and excretion is most common finding in diabetic patients. The cause is unknown, but polyuria or altered basement membranes of salivary glands were considered as the possible factors.
Oral mucosal disease
Diabetes mellitus generate chronic immunosuppression in body that may result in development of the oral mucosal diseases like lichen planus, recurrent apthous stomatitis. Coordination between physician and dentist required to treat oral mucosal diseases, which can improve the referral of patients to oral health practitioners.
Candidiasis
Immunosuppressed condition can lead to development of opportunistic infections like candidiasis. Candidiasis is a fungal infections and most commonly associated with diabetes patients. It is also associated with smoking, using unclean dentures and uncontrolled diabetes.
Taste disturbances
In patients with diabetes taste disturbances are common, taste is considered as one of the important function of oral health. According to studies, more than one-third of adults with diabetes have diminished taste perception (hypogeusia), which could result in obesity. This sensory dysfunction leads to poor glycemic regulation and abnormal diet habits.
Treatment
General physician and dentist coordination is required to treat diabetic patients with oral manifestations.
Studies have shown that treatment of periodontitis in a diabetic patients can help lower the glucose level for 3 months and doses of insulin required were reduced to half of the previous doses.
During any procedure that may require local anesthesia with epinephrine, doses of epinephrine need to be kept low as higher doses can interfere with insulin uptake and may result into hyperglycemia.
Even corticosteroids treatment can cause hyperglycemia condition and a slightly higher amount of insulin may require to control glucose level.
Presence of acute infection can also interfere with insulin uptake and that’s why slightly higher doses of medication require to control hyperglycemia during acute infections.
Conclusion
Diabetes is a non-curable disease, but with medicines hyperglycemia can be controlled. In cases of periodontitis in diabetic patients, treatment of periodontitis can help to control glycaemia and reduce the doses of drugs required. Symptomatic treatment required in case of other oral manifestations. The goal of the therapy should be to maintain the oral health in a diabetic patients. Prevalence of diabetes is increasing and awareness about oral manifestations among diabetics is essential.
References
- Nishimura F, Iwamoto Y & Soga Y. The periodontal host response with diabetes. Periodontology 2000, Vol. 43, 2007, 245–253.
- Mealey B & Ocampo G. Diabetes mellitus and periodontal disease. Periodontology 2000, Vol. 44, 2007, 127–153
- Ship J. Diabetes and oral health. An overview. JADA, Vol. 134, October 2003.
Bonus: Download our monthly e-bulletin! Click here to get it
DISCLAIMER : “Views expressed above are the author’s own.”



















Comments