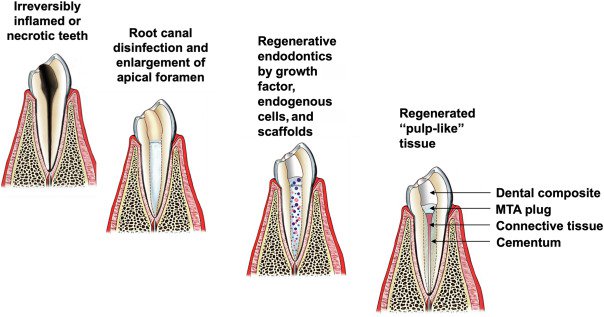
Regeneration therapy is an attractive new alternative to conventional endodontic treatments. Regenerative endodontics aims to regenerate the damaged “pulp-like” tissue, which can preserve the teeth' vitality and sensitivity while avoiding necrosis.
The cell homing technique is built on endogenous stem cells and their capacity to regenerate tissue. Cell homing refers to endogenous cells’ migration or infiltration into the site when stimulated by physiochemical or biological stimuli or by passive flow with a blood clot from the apical tissue.
The American Association of Endodontists grades a successful regenerative endodontic procedure based on 3 goals:
- Eliminate symptoms and find evidence of bony healing.
- Increased root wall thickness and root length.
- Positive response to vitality testing.
Regenerative endodontics has emerged as a promising alternative that fits mainly into the treatment of nonvital teeth, in which new pulp tissue, but not actual pulp dentin, is developed from undifferentiated cells.
There are two strategies that are applied for the pulp-dentin complex regeneration:
1. Cell-based transplantation therapy: in situ or intravenous delivery of autogenous or allogeneic stem/progenitor cell transplants.
2. Cell homing: the regeneration is accomplished via chemotaxis of endogenous host cells to the injured tissue via biological signaling molecules.
Clinically, cell homing for pulp-dentin complex regeneration might be simpler and more economical to perform compared to cell-based therapy and readily performed by clinicians without special training.
Cell Homing as a Regenerative Therapy:
Regeneration of the dental pulp tissue requires making new vital tissue in an empty and disinfected root canal space. The cell-homing technique is built on the physiological aspects of normal tissue wound healing.

Two separate cellular processes need to occur:
1. Cell recruitment and
2. Differentiation.
Cell homing therapy is initiated with the creation of bleeding by over-instrumentation.
The following blood clots filling the pulp space contain endogenous cells and growth factors necessary for tissue engineering and provide a natural structure supporting cell activity. Three terms, including revascularization, revitalization, and regeneration, are commonly used in 'regenerative endodontics’ which can be defined as follows:
- Revascularization refers to the engraftment of the regenerated pulp soft tissue to host vasculature in the root canal.
- Revitalization refers to the regeneration of hard and soft tissue.
- Regeneration refers to both revascularization and revitalization, including dentin and root structure as well as cells of the pulp-dentin complex.
Three aspects necessary for tissue regeneration are :
- Stem Cells
- Growth Factors
- Biomaterials/Scaffolds.
Stem Cells
Clinically, most cells in a treated root canal would be surgically removed by extirpation or chemically destroyed by endodontic disinfection agents. New cells and stem cells must either be transplanted to the root canal space or recruited from the apical papilla (Stem Cells from Apical Papilla, SCAP).
Cell homing techniques specialize in recruiting SCAPs for pulp regeneration.
Favorable characteristics of SCAPs:
- Differentiate without exogenous growth factors.
- Show less telomere shortening compared to other mesenchymal stem cells.
- SCAPs from the apical papilla of immature teeth are highly proliferative and capable of differentiating into “odontoblast-like” cells.
Growth factors:
Growth factors are polypeptides or proteins that, when bound, give rise to a broad range of cellular activities such as migration, proliferation, differentiation, and maturation. Modulating specific signaling pathways makes growth factors essential in tissue reparation and regeneration.
There are two types of growth factors involved in the process:
- Exogenous
- Endogenous
Recent studies have found regeneration to occur without using exogenous growth factors. Endogenous growth factors include Dentine Derived Growth Factors(DDGF) like transforming growth factor Beta 1, angiogenic growth factors, etc.
Growth factor concentrates can be made from the recipients' own blood and injected into the root canal to further enhance regeneration.
Biomaterials/Scaffolds
A successful scaffold should give structural support for colonizing cells, promoting cell survival, proliferation, and differentiation, and promoting cell interactions such as adhesion and deposition of extracellular matrix.
To fully regenerate tissue, the scaffold should be degradable at a rate adapted for tissue healing. Mixing the scaffold with chemical agents, growth factors, and cells will modify the scaffold and raise its conductive potential.
Fibrin has been a widely used scaffold design in tissue engineering for its advantages:
- Can be made from the patient's own blood, limiting the risk of foreign body reaction and infection.
- Is highly versatile and can be produced in different designs, such as injectable hydrogels or microbeads.
Conclusion
Regenerative endodontics has the potential of revitalizing necrotic teeth as well as securing continued root formation and root thickening in immature teeth. Tooth sensitivity and a remaining solid tooth substance reduce the fracture risk and tooth loss. A vital tooth also can defend itself from foreign invaders.
The cell-homing approach of regenerative endodontics shows promising results that can be translated into clinical practice.
Source: https://www.sciencedirect.com/


















Comments