Introduction
Among lesions in the oral cavity consisting of abnormal growths, pyogenic granuloma is the most common, even in children. ‘Pyogenic granuloma’ is a misleading term as they are neither infectious nor granulomatous. The correct name for it would be – lobular capillary hemangioma. This lesion usually occurs in children and young adults as a solitary, shiny red papule or nodule, prone to bleeding and ulceration.
- Name: Azmi
- Age/Gender: 9 yrs/female
- Place of birth: Amroha
- Address: Amroha UP
- Parent’s occupation: Father is a farmer, mother is a housewife.
- Religion: Muslim
- Family income: 4 figures
Case Report
A 9 year old female patient reported to the clinic with a chief complaint of bleeding gums and bad breath since 1-2 months.

The patient was completely asymptomatic 1-2 months back. She noticed a small swelling on the lingual side of her lower anterior region. The swelling gradually increased in size and also developed a tendency to bleed.
Nothing relevant was reported in pre-natal, natal and post natal history.
On extra oral examination, no abnormality was detected in hairline, skin, eyes, nose, ears, lips, nails, lymph nodes and TMJ.
On intra oral examination, a gingival overgrowth was seen irt 73, 74, 75 which was soft in consistency and was bleeding on slight touch. Deep carious lesions were seen in 64. The dentition was mixed dentition, with a Class I molar relationship on both the sides. The overjet and overbite were normal. No abnormality was detected on rest of the soft tissue.



Intra Oral Examination: Mucosa, Palate, Floor of the Mouth, Tongue, Salivary Gland, Lymph Nodes and Buccal Mucosa.
Gingiva: Pale pinkish in color scalloped with round margins
- Teeth present: 16 55 54 53 12 11 21 22 63 64 65 26 36 75 74 73 32 31 41 42 83 84 85 46
- Stains/Calculus: +/+
- Carious 64
- MOLAR RELATIONSHIP: Angle’s Class 1 (on both sides)
- Overjet/Overbite: Normal
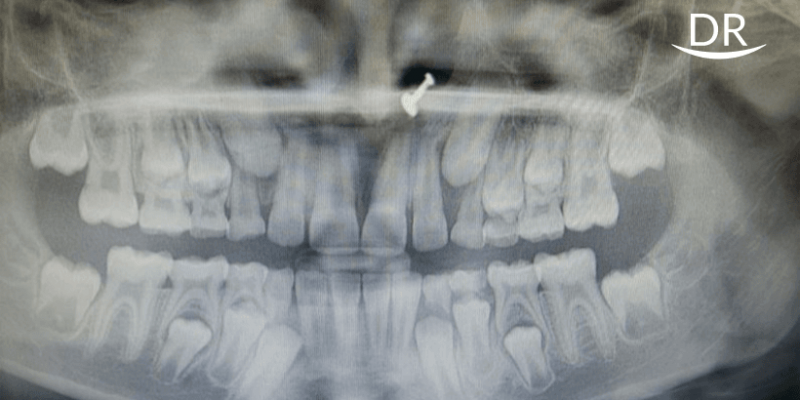
Provisional diagnosis was pyogenic granuloma. An orthopantomogram (OPG) was taken.

The differential diagnosis was
- peripheral giant cell granuloma (presence of multinucleated giant cells and lack of an infectious source)
- peripheral ossifying fibroma (minimal vascular component unlike a pyogenic granuloma)
- pregnancy tumour
- Kaposi’s sarcoma (acquired deficiency syndrome)
For the final diagnosis, an excisions biopsy was planned
Provisional diagnosis: Pyogenic Granuloma
Investigation: OPG was done
Differential Diagnosis:
Treatment Plan
For the preparatory phase oral prophylaxis and oral hygiene instructions were given. The patient was sent for minor blood investigations – CBC, CT, BT.
For the corrective phase, surgical excision of the overgrowth and extraction of 64 was done. Patient was kept on a periodic recall and follow up for every 3 months.
Corrective Phase
Extraction of 64 was done. For the surgical excision –
- Intra oral and extra oral scrubbing was done with betadine solution
- Gingival incision was given with scalpel blade
- The gingival tissue was obtained and sent for biopsy


The biopsy result and the final diagnosis was pyogenic granuloma.

Discussion
Pyogenic Granuloma (PG) (also known as "Granuloma gravidarum") is primarily an oral disease which was first described by Hullihen in 1844 and was originally described in 1897 by two French surgeons, Poncet and Dor, who named this lesion as “OtyomycosisHominis.” It is actually not a granuloma but a capillary haemangioma due to which it has the inherent tendency to bleed. This term was introduced by Hartzal in 1904.
The etiology of pyogenic granuloma is generally multifactorial and various factors are responsible for its occurrence. They can be briefly summarized as
- alterations of the physiologic bio-hormonal cycles
- presence of generalized reactive hyperplasia of gingival mucosa
- presence of infective centres of tissues surrounding the dental elements
- subjective features of periodontium (typical in pregnancy)
- pharmacologic therapy (oral-contraceptive pills & immuno-suppressant drugs
This type of growth is typically seen in young adults although it may occur at any age, especially in individuals with poor oral hygiene. The lesion varies from a discrete, spherical, tumour like mass with pedunculated attachment with flattened, keloid like enlargement with a broad base. It appears to involute spontaneously to become a fibro epithelial papilloma, or it may persist as unchanged tissue for many years.


The size of pyogenic granuloma varies from 2 mm to 2 cm in diameter. Sometimes, the lesions may reach a diameter up to 5 cm also. In majority of cases, it affects the gingiva but may also occur on the lips, tongue, oral mucosa and palate.
There is a marked variation in the appearance of the lesion, ranging from red/pink to purple. Younger lesions are likely to be red because of large number of blood vessels. Older lesions become pink.
Histopathologically, PG shows a highly vascular proliferation resembling granulation tissue. Numerous small and large endothelium lined blood vessels engorged by red blood cells are often seen. The channels are often organised in a lobular arrangement thus deriving the term “lobular capillary hemangioma (LCH)”. Some pathologists consider it as a polypoid form of capillary hemangioma or an inflamed lobular hemangioma while others consider it as granulation tissue type hemangioma.
Two histologic variants of PG have been described: LCH and nonlobular capillary hemangioma (non-LCH).
- The first type has proliferating blood vessels arranged in lobular aggregates although there may not be any edema, capillary dilation or granulation tissue proliferation
- The non-LCH has a highly vascular proliferation resembling granulation tissue
- Varying degrees of inflammatory cells infiltrate are seen in both types
Differential diagnosis & how to differentiate PG from other lesions – It is very important to differentiate this growth from various other lesions that occur in the oral cavity. These include
- peripheral giant cell granuloma
- peripheral ossifying fibroma
- metastatic cancer
- Haemangioma
- pregnancy tumour
- conventional granulation tissue hyperplasia
- Kaposi’s sarcoma
- bacillary angiomatosis
- non Hodgkins lymphoma
Peripheral giant cell granuloma can be distinguished on the basis of histopathological examination due to the presence of multinucleated giant cells and lack of an infectious source.
Ossifying fibroma or peripheral odontogenic fibroma has a minimal vascular component unlike a pyogenic granuloma.
Due to the proliferating blood vessels, differential diagnosis of pyogenic granuloma from a hemangioma is made histologically. Hemangioma shows endothelial cell proliferation without acute inflammatory cell infiltrate, which is a common finding in pyogenic granuloma.
Metastatic tumours of the oral cavity are rare and attached gingiva is commonly affected. While clinically they resemble reactive or hyperplastic lesions such as pyogenic granuloma, microscopically they usually resemble the tumour of origin, which usually is distant from the metastatic lesion seen in the oral cavity.
Pyogenic granuloma is distinguished from Kaposi’s sarcoma in Acquired Deficiecy Syndrome by to the proliferation of dysplastic spindle cells, vascular clefts, extravasated erythrocytes and intracellular hyaline bodies, none of which are seen in pyogenic granuloma.
Management of pyogenic granuloma is conservative surgical excision, after thorough oral prophylaxis.
- If the lesion is small, painless and free of bleeding, oral prophylaxis and removal of causative irritants is advised
- If the lesion is of large size, a thorough oral prophylaxis followed by surgical excision using gingivectomy or flap surgery procedures is done
- Other treatment protocols have also been proposed such as cryosurgery which is safe, easy and inexpensive; and also Nd: YAG and CO2 and flash lamp pulsed dye lasers. Lasers have advantage of minimum pain and invasiveness and the lack of need for suturing or packing
Besides excision, lasers can be used for frenectomy too. Click here to read a case of lingual frenectomy using a diode laser.
Conclusion
The correct evaluation of pediatric patients before the biopsy is fundamental for better management of children with pyogenic granuloma. The use of electrocautery and lasers provide a new tool that can modify the way in which the present treatments are being performed, or serve to compliment them.
References
- Shafer’s Textbook of Oral Pathology
- Trivedi S. Capillary hemangioma or pyogenic granuloma. Indian Society of Periodontology. 2016
- daSilva FC, Piazzetta CM, Torres‑Pereira CC, Schussel JL, Amenábar JM. Gingival proliferative lesions in children and adolescents in Brazil: A 15-year-period cross-sectional study. Indian Society of Periodontology. 2016
- Singh B. Laser therapy – a promising approach for managing Pyogenic Granuloma – A case report. Clinical dentistry. 2015
- Buchner A, Shnaiderman A, Vared M. Pediatric localized reactive gingival lesions: A retrospective study from Israel. Pediatr Dent 2010; 32:486-92



















Comments