
A Brief Highlight on Osteoporosis
In the 1930s, osteoporosis was defined as “too little calcified bone”.1 More recently, osteoporosis has been used to refer anatomically to a condition of generalized reduction in bone mass with no other abnormality.2 Osteoporosis is a systemic skeletal condition diagnosed based on the bone mineral density with bone densitometry. Osteoporosis results in increased bone turn over. The rate of bone resorption exceeds the bone formation rate thus leading to bone loss. Osteoporosis is common in post-menopausal women. The condition increases bone fragility and the risk of bone fracture is high. Osteoporosis affects the quality of life and increases morbidity.3

Bone Metabolism in Osteoporosis
It is generally believed that bone loss may be the result of an abnormal accentuation of the disequilibrium between bone resorption and formation, resulting from a decrease in bone formation, an increased bone resorption, or a combination of the two.4 Although this may be true for some patients with osteoporosis, the disease is also characterized by anatomic and histopathogenetic heterogeneity, with different disturbances in bone remodelling at the organ tissue and cell levels, leading to the same syndrome.5
The process of remodelling involves the constant removal and replacement of bone tissue, which contributes to the skeleton’s ability to resist load without suffering fatigue damage. The rates of bone loss or gain at particular sites and times are controlled by the speed and scope of the replacement. Although bone remodelling may be hyperkinetic and lead to accelerated bone loss in some osteoporotic patients, the process is low or normal in most patients. This has been confirmed by bone histomorphometry, which is accepted as the only method that provides a direct precise analysis of the static and dynamic cellular and tissue abnormalities.5
Iliac crest biopsy specimens have shown bone turnover to be high in about 25%, normal in about 45%, and low in about 30% of patients.6 From an analysis of 154 iliac bone samples, Meunier et al. reported that “there are 48% of the patients without detectable abnormality of remodelling surfaces and appositional rate at the time of the biopsies”; only 33% of the patients had trabecular osteoclastic resorption surfaces higher than two standard deviations above the normal.7
Concept of Osseointegration
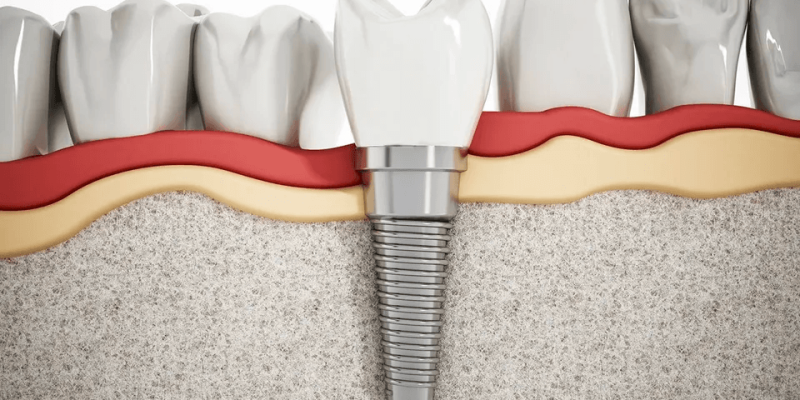
Osseointegration is defined as “a direct structural and functional connection between ordered living bone and the surface of a load-carrying implant.”8 An implant is osseointegrated when it is in direct contact with the bone, and there is no relative movement between the implant and the bone. In other words, osseointegration is expressed clinically as long term state of stability of the implant in the vital bone.
The cellular response after implantation depends on implant surface characteristics, the stability, and heating injuries of the host bone. Bone healing around implants involves a cascade of cellular and extracellular biological events (like fracture healing) until the entire implant surface is embedded in bone:
- The first biological component to contact the implant surface is blood and blood cells from the surrounding vasculature.
- These blood cells are activated and release cytokines and other growth and differentiation factors on and around the implant.
- Platelets undergo biochemical and morphological changes due to contact with the implant surface and undergo adhesion, spreading, and aggregation.
- They induce phosphotyrosine, increase intracellular calcium, and cause hydrolysis of phospholipids to form a fibrin matrix that regulates cell adhesion and binding of minerals.
- This matrix is a calcified afibrillar layer consisting of osteoid and lamina limitans (organic layer) that is rich in calcium, phosphorus, osteopontin, and bone sialoprotein.9
- This matrix acts as a scaffold for osteogenic cells to migrate and differentiate to form osteoid and trabecular bone (osteoconduction), which will ultimately remodel to form lamellar bone around the implant surface.

Chances of implant failure
Implant failure is manifested as implant mobility. Early implant failure occurs due to poor bone – implant surface contact. Interruption of osseointegration due to over loading can also cause implant failure.10 Osteonecrosis induced by Bisphosphonates (BRONJ-explained below) results in implant failure due to reduced bone turn over. However, Osteonecrosis commonly occurs in patients under i.v Bisphosphonates. Systemic diseases, steroids, immunosuppressant, trauma, and poor oral hygiene are the trigger factors for osteonecrosis.11
Treatment for Osteoporosis – Bisphosphonates
Bisphosphonates are the drug of choice for Osteoporosis. Bisphosphonates are being used for the past 40 years for treatment of Osteoporosis, Paget’s disease, and few other conditions. Bisphosphonates reduce the osteoclastic activity and suppress bone remodelling and turnover.10
The mechanism of action of Bisphosphonates is that they accumulate in the osteoclastic sites of the bone due to its high affinity for bone minerals.The Bisphosphonates are then incorporated into the osteoclastic cells and bone resorption is interrupted. The number of osteoclasts is also reduced thus decreasing bone resorption. The aim of bisphosphonates is to achieve normal bone remodelling level.12 Bisphosphonates remain in the bone for years and have a long-lasting effect. Bisphosphonates also cause delayed wound healing due to reduction in collagen expression by the fibroblasts. Prolonged usage of Bisphosphonates might lead to adverse effects such as Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ).13
Implants in Osteoporosis with Bisphosphonates
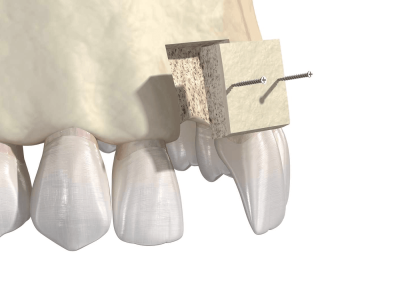
Osseointegration is percent contact between surface of implant and bone. Prognosis of dental implants is not only dependent on implant placement and the surgical procedure. It is also determined by the patient factors such as bone quality and systemic health. Certain experimental model suggests that osteoporosis affects osseointegration.10 However literature states that patients with osteoporosis do not appear to be at significant risk of implant failure. Osteonecrosis of the jaw is the adverse effect of Bisphosphonate therapy. Frequently patients under i.v Bisphosphonate therapy for malignant diseases are affected with osteonecrosis. Osteoporosis is treated with oral Bisphosphonates and hence not a contraindication for dental implant placement.14
How Osteoporosis Can Lead to Dental Implant Failure
Osteoporosis is a major systemic condition, which adversely affects osseointegration and implant survival. Few findings showed that osteoporotic conditions alter peri-implant bone characteristics after implant osseointegration, the involved mechanism remains unclear. It can be assumed that osteoporosis affects osteoblast/osteoclast proliferation and activity in the vicinity of titanium implants.15 Specifically, post estrogen deficiency can induce an imbalance in the expression of several molecules and cell receptors (e.g., RANKL and OPG), resulting in peri-implant bone alterations.
Clinically, August et al. previously reported a higher rate of implant loss (13.6%) in the maxilla of osteoporotic women without antiosteoporosis treatment compared with patients with treatment (6.3%, p = 0.039).16
Furthermore, it must be emphasized that it is not clear whether the osteoporotic process can be reversed and the amount of bone after osteoporotic therapy will increase again. Therefore, it is recommended that more research is conducted toward this phenomenon considering the still-increasing numbers of dental implants applied to an aging world population.

Conclusion
Osteoporosis does not preclude a patient from receiving dental implants. Oral bisphosphonates have a low risk of osteonecrosis. Prior to the procedure, the patient must, however, be informed of their systemic condition and give their informed consent. Patients seeking dental care should not be denied implant treatment options due to osteoporosis. Benefit to the individual: Risk assessment will produce a prognosis that is predictable.
References
1. Nordin BEC. The definition and diagnosis of osteoporosis. Calcif Tissue Int 1987;40:57-58.
2. Harrison JE. Osteoporosis. In: Tam CS, Heersche JNM, Murray TM (eds.) Metabolic Bone Disease: Cellular and Tissue Mechanisms. Boca Raton: CRC Press, 1989:240-267.
3. Mellado-Valero A, Ferrer-García JC, Calvo Catala J, Labaig-Rueda C. Implant treatment in patients with osteoporosis. Med Oral Patol Oral Cir Bucal.1; 15:e52-7 (2010).
4. Nordin BEC, Aaron J, Makins N, Francis R, Sagreiya K. Bone formation and resorption in postmenopausal osteoporosis. In: Dixon ASJ, Russell RGG, Stamp TCB (eds). Osteoporosis: A Multidisciplinary Problem. London: Royal Society of Medicine, 1983:161-171
5. Meunier PJ. Assessment of bone turnover by histomorphometry in osteoporosis. In: Riggs BL, Melton LJ (eds). Osteoporosis: Etiology, Diagnosis, and Management. New York: Raven Press, 1988:317-332.
6. Riggs BL, Melton LJ. Involutional osteoporosis. New Engl J Med, 1986;314:1676-1686.
7. Meunier PJ, Briançon D, Sellami S, Edouard C, Chavassieux P, Arlot M. Dynamic bone histomorphometry in primary osteoporosis. In: Dixon AStJ, Russell RGG, Stamp TCB (eds). Osteoporosis: A Multidisciplinary Problem. London: Royal Society of Medicine, 1983:67-73.
8. BranEmark PI. Introduction to osseointegration. In: BraNemark PI, Zarb G, Albrektsson T, editors. Tissue integrated prostheses. Osseointegration in clinical dentistry. Chicago and Tokyo: Quintessence; 1985. p. 350.
9. Stanford CM, Keller JC. The concept of osseointegration and bone matrix expression. Crit Rev Oral Biol Med. 1991;2(1):83–101
10. Ballantyne E “Bisphosphonates: Possible Modes of Action and Implications for Dental Implant Treatment. A Review of the Literature.” J Gen Pract; 3: 192 (2014).
11. Kwon TG, Lee CO, Park JW, Choi SY, Rijal G, et al. Osteonecrosis associated with dental implants in patients undergoing bisphosphonate treatment. Clin Oral Implants Res 25: 632-640 (2014).
12. Pedro Diz, Dental implants in the medically compromised patient. Journal of Dentistry; 41 : 195–206 (2013).
13. Javed F, Almas K. Osseointegration of dental implants in patients undergoing bisphosphonate treatment: a literature review. J Periodontol. ; 81:479–84 (2010).
14. Giro G, Chambrone L, Goldstein A, Rodrigues JA, Zenóbio E, Feres M, Figueiredo LC, Cassoni A, Shibli JA. Impact of osteoporosis in dental implants: A systematic review. World J Orthop; 6: 311-315 (2015).
15. Marco, F.; Milena, F.; Gianluca, G.; Vittoria, O. Peri-implant osteogenesis in health and osteoporosis. Micron 2005, 36, 630–644.
16. August, M.; Chung, K.; Chang, Y.; Glowacki, J. Influence of estrogen status on endosseous implant osseointegration. J. Oral Maxillofac. Surg. 2001, 59, 1285–1289.


















Comments