Abstract
Discover a comprehensive guide on dental implant systems, including how to choose the best products for your practice. Learn about titanium grades, their properties, and factors to consider when selecting implants, abutments, and clinical screws.
Keywords dental implant systems, titanium grades, implant selection, abutments, clinical screws, dental practice, implant compatibility, implant materials, dental implant products, implant performance
Introduction
Dental implant systems are a vital component of modern dental practices. Choosing the right system can enhance patient outcomes and streamline dental work. This guide aims to help dentists make informed decisions about products not only by studying the characteristics and assurances of manufacturers, but also by considering the reliability of the supplier and the availability of all options in stock. It is also very helpful if the manufacturer provides test kits for testing, which indicates that the manufacturer is confident in the quality of their products. We will also discuss some less obvious criteria for selection.
Choosing an implant system based on materials used for implants, abutments and clinical screws
Various types of titanium and titanium alloys are used for dental implants, abutments, and clinical screws. The three most common grades are. Each type of titanium grade used in dental implants, abutments, and clinical screws has unique characteristics that affect their performance and biocompatibility. Here’s a detailed description of each grade:
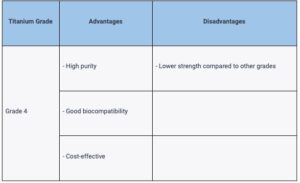
Grade 4 Titanium
Grade 4 Titanium, also known as commercially pure titanium (CP titanium), is the purest form of titanium used in dental applications. It has a high level of biocompatibility and is more cost-effective than other grades. However, it has lower strength compared to titanium alloys such as Grade 5 and Grade 23.
Grade 5 Titanium
Grade 5 Titanium (Ti-6Al-4V), also known as Ti-6Al-4V, is an alloy made up of titanium combined with 6% aluminum and 4% vanadium. This combination increases its strength-to-weight ratio, fatigue resistance, and wear resistance. However, it has slightly lower biocompatibility compared to Grade 4 due to the presence of alloying elements and is more expensive.
Grade 23 Titanium
Grade 23 Titanium (Ti-6Al-4V ELI), also known as Ti-6Al-4V ELI (Extra Low Interstitial), is a variant of Grade 5 titanium with reduced levels of interstitial elements like oxygen, nitrogen, and carbon. This results in superior biocompatibility, high strength, and excellent fatigue resistance. However, it comes at a higher cost compared to other grades. Strength and resistance to elastic deformation are especially important for clinical screws, as their thickness is slightly over 1 mm. In addition, Grade 23 alloy surpasses Grade 5 in terms of ductility and resistance to elastic deformation by 5-15%, depending on the production technology and method of processing final parts. At first glance, the difference may seem insignificant, but sometimes such a difference can be the cause of a screw failure or a crack in the coronal part of the implant.
Comparison table:
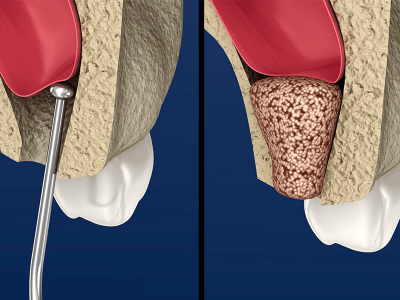
Choosing an implant system based on surface treatments
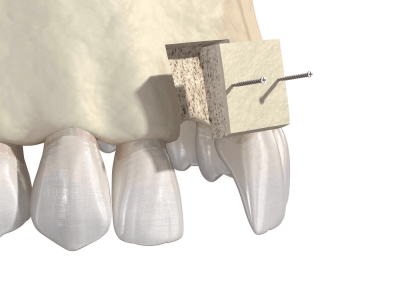
Each method of treating the surface of dental implants has unique characteristics that affect osseointegration and bone contact with the implant. A rough surface on a titanium implant integrates much better with bone tissue cells. The difference between a smooth (milled) and modified surface can be seen under a microscope in the illustration below.

Unmodified (left) and modified titanium surface (right) under a microscope
Surface modification can be achieved through various methods. Here are descriptions of some of the most popular methods:
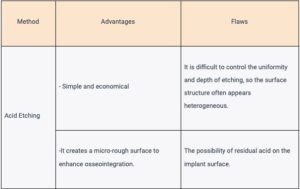
Acid Etching
Acid etching involves immersing the dental implant in an acid solution to create microscopic pits and irregularities on the implant surface. This process increases the surface area and improves bone contact with the implant. However, it is now used less frequently and considered outdated due to the unevenness and unpredictability of the structures created on the implant surface.
Anodization
Anodization is an electrochemical process that creates a controlled oxide layer on the surface of the dental implant. This oxide layer can be regulated to create a range of surface roughness levels, which can improve the biocompatibility of the implant and promote osseointegration. However, controlling the electrochemical process of anodization can be difficult, resulting in unpredictable outcomes. Additionally, the high cost of implementation hinders its widespread use.
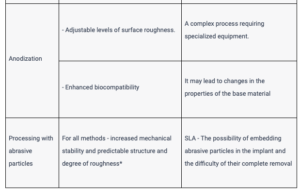
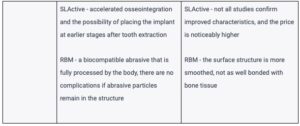
Abrasive particle treatment (SLA, SLActive, RBM)
These are the most effective treatment methods and are therefore most widely used. The surface is treated with a stream of abrasive particles at high speed, and the differences between these processes are as follows:
- SLA (Sandblasted, Large-grit, Acid-etched) – the surface is treated with a stream of hard abrasive particles made of aluminum oxide. Acid etching is then applied, but the main purpose of the acid treatment is not to modify the surface, but to remove trapped abrasive fragments. The result is a homogeneous structure with a specified degree of roughness. However, it is not always possible to remove 100% of the abrasive particles, which sometimes slows down osseointegration.
- SLActive – the process is similar to SLA technology, but an additional step of treatment in an inert environment is added at the end. This stabilizes the surface structure and moistens it. Such implants are supplied in sterile packaging filled with saline. This improved treatment version allows for faster healing. Under the most favorable conditions, the osseointegration process occurs 30-50% faster. However, not all studies confirm such good efficacy. The price of implants modified using the SLActive technology is noticeably higher compared to those treated with the SLA method.
- RBM (Resorbable Blast Media) – the method is different. Biocompatible material particles, such as sodium bicarbonate or calcium phosphate (hydroxyapatite), are used as the abrasive. The hardness of these particles is less compared to aluminum oxide. Therefore, the surface obtains less pronounced irregularities. However, the surface structure is still porous enough to accelerate the osseointegration process. This method has several key advantages:
- the cleaning procedure after sandblasting is simplified – aggressive acids are not needed to remove abrasive particles;
- if abrasive particles remain on the surface, they dissolve and are used by osteocytes as building material, which accelerates the osseointegration process.
Comparison table:
When choosing, ask if tests were conducted on the surface condition:
- how much pure titanium is on the contact surface;
- carbon and other impurities.
Choosing an implant system based on surface roughness
One important characteristic of surface quality is the degree of roughness, which is determined by the height of peaks and valleys on the implant surface and denoted as ‘Sa’. Specialists categorize four groups based on the degree of roughness:
- smooth – Sa < 0.5 μm – these milled surfaces for direct contact with bone are not currently used;
- minimally rough – Sa = 0.5 – 1.0 μm;
- moderately rough – Sa = 1.0-2.0 μm – the optimal option for modern dental implants;
- highly rough – Sa > 2.0 μm – used in specific cases.
Request and verify these indicators from dental implant manufacturers.
Choosing an implant system based on abutment-to-implant interface
Popular abutment-implant interfaces include:
- External hexagonal connection – has high strength, especially under lateral loads, but insufficient sealing at the implant/abutment connection line.
- Internal hexagonal connection – one of the most common standard interfaces.
- Tapered (Morse taper) connection – has the best sealing at the implant/abutment line, almost no fluid passes into the internal structures.
Standardization of these interfaces ensures compatibility between components from different manufacturers, making it easier for dentists to find spare parts. We do not recommend choosing implant systems with exclusive interfaces. Over time, the manufacturer may discontinue this interface or even disappear from the market. And if the patient needs to replace the abutment, it will be extremely difficult to do so.
Mistakes to avoid when choosing a dental implant system
Some common mistakes to avoid include:
- Prioritizing price over quality
- Failing to consider the supplier’s reliability, delivery times and stock availability
- Neglecting to research product reviews and consult professional opinions
FAQ: Choosing the right dental implant system for your practice
What factors should I consider when comparing different dental implant materials?
When researching different titanium grades for dental implants, consider
- biocompatibility
- strength
- fatigue resistance
- wear resistance and
- cost.
How do various surface treatment methods impact the performance of dental implants?
Surface treatments like acid etching, anodization, blasting, and plasma spraying affect the implant’s osseointegration, bone-to-implant contact, and biocompatibility.
Why is it important to consider abutment-to-implant interfaces when selecting a dental implant system?
Standardized abutment-to-implant interfaces allow for compatibility between components from different manufacturers, making it easier to source replacement parts and providing flexibility in your dental practice
If the price isn’t the sole indicator of quality, how can I determine the value of a dental implant system?
Examine product specifications, research the materials and surface treatments used, and consult reviews from professionals who have experience using the products.
What factors should I prioritize when choosing a supplier for dental implant systems?
Prioritize supplier reliability, consistent market presence, fast delivery times, and their willingness to accept returns for unsuitable items.
How can I evaluate the quality of a dental implant system before committing to a purchase?
Utilize trial kits provided by the manufacturer or supplier to assess product quality, functionality, and compatibility with your dental practice’s needs.
To conclude
In conclusion, choosing the right dental implant system is crucial for your practice’s success. By considering factors such as materials, surface treatments, interfaces, pricing, supplier reliability, and product evaluations, you can make informed decisions and provide the best possible care for your patients.
References
- https://www.nature.com/articles/s41598-021-93307-4
- https://www.sciencedirect.com/science/article/pii/S246849882100010X
- https://www.researchgate.net/publication/349211791_Which_dental_implant_surface_is_more_effective_in_osteointegration_RBM_surface_versus_SLA_surface
- https://www.mdpi.com/2673-1592/2/2/11



















Comments