Abstract
Successful implant dentistry can be directly co-related to quality and quantity of bone at the recipient site of implant. The use of bone grafts for management of various osseous defects has been available for many years. Interest in bone reconstruction for the oral cavity has increased dramatically over the past decade with widespread acceptance of dental implant. Many patients who request implant rehabilitation require ancillary procedures to increase the quantity and quality of their recipient bone.Bone has an internal structure described in terms of quality which reflects the strength of bone. The density of available bone in an edentulous site is a determining factor in treatment planning, implant design, surgical approach, healing time and initial progressive bone loading during prosthetic reconstruction.Atrophy of the alveolar processes is expressed as reduction of height and width. This review provides a contemporary and comprehensive information about various bone graft used in dental implant management.
Keywords: Dental implants; bone grafts; graft material

Introduction
Many patients who request implant rehabilitation require ancillary procedures to increase the quantity and quality of their recipient bone. [1] Bone has an internal structure described in terms of quality which reflects the strength of bone. Atrophy of the alveolar processes is expressed as reduction of height and width. The density of available bone in an edentulous site is a determining factor in treatment planning, implant design, surgical approach, healing time and initial progressive bone loading during prosthetic reconstruction. [2-4]
Healing of bone grafts
Incorporation of the grafts happens in concert with a process of initial remodelling and resorption, which is associated with a loss of bone volume. The amount and rate of this resorption depends on many factors, such as
- dimensions of bone graft
- quality of recipient site
- biomechanical properties and
- fixation to surrounding bone.[5]
Graft healing occurs in one of 3 ways: osteogenesis, osteoinduction or osteoconduction. The proportion of these processes in each case depends largely on type of graft and conditions of host site(s).
Osteogenesis occurs when the graft itself supplies viable osteoblasts (osteogenic cells) as the source of new bone. It is well known that bone source (for instance, the iliac crest) with high proportions of marrow have better osteogenic properties due to all increased number of in differentiated cells.[7] During healing phase of graft there is competition between bone-forming cells and soft-tissue-forming cells to fill the defect.[8]
The graft is replaced in a period that lasts between 3 to 6 months. When this occurs the hypervascularity gradually disappears.[6] There is a histological response running parallel to vascular one. Granulation tissue with fibroblastic and angioblastic proliferation is followed by proliferation of immature osteoid tissue at periphery of graft. After the osteoid is replaced by mature bone there is no evidence of grafted avascular bone graft.
Classification of grafts
Bone grafts can be classified according to the structure, source and immune response and embryological origin.
Bone grafts classified according to structure include [9,10]:
- Cortical skull, chin and body of mandible
- Cancellous – Inner tibia or iliac crest
- Cortico- cancellous or composite- Blocks from iliac crest
Bone grafts classified according to source and immune response include:
- Autograft or autologous
- Autograft- from a different human
- Xenograft- from another living being
- Alloplast or Synthetic
Bone grafts classified according to embryological origin include:
- Membranous: originated from mesenchymal cells (for instance, all the bone located in the craniofacial skeleton)
- Endochondral- originated from ectomesenchymal cells (for instance, iliac crest, tibia)
Cortical Bone
This type of bone is highly osteoconductive due to Haversian system and thus more resistant to resorption, which is useful when structural rigidity is an issue. It is, however, deficient in osteogenic cells.
Cortical bone can be harvested in large quantities from the parietal bones. The problem of medium-sized defects can be solved with blocks from chin, body and ramus of mandible. The zygomatic buttress is more suitable for small defects or dehiscence.[11]
The gold standard for bone reconstruction is fresh autograft. Among different autologous sources, cancellous bone from iliac crest has been considered the reference source, due to its enhanced osteogenic properties.
General Principles of Bone Grafting
Preservation:
One of the main goals when harvesting bone grafting is preservation of highest possible number of living osteoblasts.
Sterility must be preserved from removal of the graft until delivery at the recipient site.
Once removed it can be kept enveloped in moist gauze. This can be soaked with isotonic serum or, even better, with autologous blood or platelet- rich plasma (PRP). Soaking the graft in saline may accelerate cell lysis. Some authors recommend embedding graft with antibiotics to protect it until revascularisation takes places.[12]
Trimming:
In most instances, grafts need to be adapted to defective area. The proportion of cortical bone (rigidity) of the graft usually correlates with the difficulty in adaption to the host site.[13]
Cancellous bone is usually condensed and applied with the aid of sterile syringes or bones carriers into a cavity or space (for instance, maxillary sinus). For better handling of cancellous or particulated grafts we strongly recommend the use of PRP as a ‘biological’ carrier.This mixture gives stability to graft and facilitates manipulation and delivery to recipient site. Through use of PRP as a ‘carrier’, the transport and adaption of particulated grafts have become much easier. Cortical and composite blocks need to be adequately adapted and fixed to recipient site in order to allow incorporation. Big grafts from the iliac crest or calvarium usually need to be cut into different pieces before adaption.[14]
Before the harvesting procedure, it is of the utmost importance to determine accurately the shape and size of grafts needed in order to limit morbidity and avoid wasting material. Saws, burs and rongeurs are necessary to trim the blocks, and if particulate bone is needed for specific reconstruction, it might also be necessary to grind cortical blocks with a bone mill.
Recipient site:
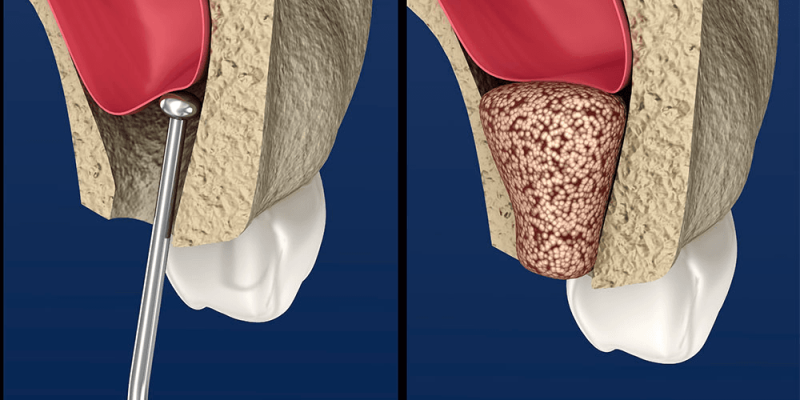
Preparation of the recipient site includes adequate periosteal elevation and peeling of all fibrous remnants inserted in or adherent to bone.
To ‘activate’ the recipient bed we recommend performing small perforations in cortex with a fissure bur. This seems to facilitate vascular and tissue in-growth from the medullary area in host bone into graft.[15]
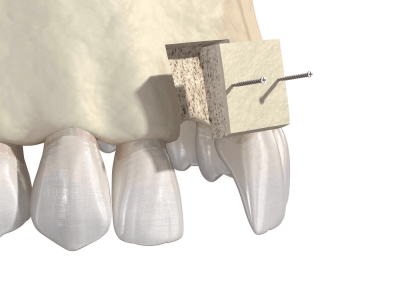
Harvesting and Fixation
In most cases a single screw will suffice to stabilise those from the iliac crest, which often requires ‘flexible’ adaption, may need two or more screws to achieve perfect stabilisation of the graft. The screws should act in a compression fashion- that is, the hole in graft should be bigger than the screw. This way the shaft of the screw will circulate freely through graft and the head of screw will compress the block against recipient site.[12]
Screws with a diameter of 1.5 mm or 20 mm are currently used for graft fixation. Rigid fixation is mandatory for graft survival and compression screws are the best way to achieve it. There are instances where screw fixation is not possible and either wire or suture fixation can be applied so that graft is protected from loading during healing period.[16,17,18]
Harvesting and Fixation instruments:
Bone grafting requires a specific armamentarium that varies according to the donor site.
Intra-Oral Harvesting:[19-24]
There is a specific armamentarium for bone harvesting, depending on the donor site.
Bone-Cutting Instruments:
The ideal bone cutter should be fast, easy to handle and atraumatic as possible.
- Saws (reciprocating and oscillating) are ideal in cases where this cuts are necessary. The drawbacks are difficulties in reaching certain areas of oral cavity, cost and the fact this cuts do not allow chisels to get in.
- Tissue burs are used for corticotomies and round lab burs for grafts remodelling. They are very effective, easy to handle and cheap.
- Discs are dangerous unless guarded. They can easily ‘run’ into the soft tissues causing lacerations. They are ‘cheap’ alternative to saws.
- Rongeurs are excellent for harvesting and/or cutting bone from the tuberosity areas. They bite soft bone very atraumatically.
- Chisels are good as osteotomes in the maxilla. They should not be used in mandible-at least not maleated- to avoid trauma to TMJ. They are effective in ‘elevating’ bone grafts once corticotomes have been completed.
- Bone – milling devices: There are several companies producing such instruments. A sharp bone rongeurs can be a good substitute.
Conclusion
In the present era of dentistry, autologous bone grafts remain the prime preference in most of the cases. Different bone replacement grafts from other sources that possess different properties are also available as alternate options. With various available grafts and regenerative techniques, extensive knowledge of the principles, harvesting & healing of these grafts is the cornerstone of successful regeneration. Adapting these guidelines can be advantageous to achieve successful treatment outcomes.
References
1. Ananth H, Kundapur V, Mohammed HS, Anand M, Amarnath GS, Mankar S. A Review on Biomaterials in Dental Implantology. Int J Biomed Sci. 2015 Sep;11(3):113-20.
2. Oshida Y, Tuna EB, Aktören O, Gençay K. Dental implant systems. Int J Mol Sci. 2010 Apr 12;11(4):1580-678.
3. Tonelli P, Duvina M, Barbato L, Biondi E, Nuti N, Brancato L, Rose GD. Bone regeneration in dentistry. Clin Cases Miner Bone Metab. 2011 Sep;8(3):24-8.
4. Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS, Koval KJ. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J Orthop Trauma. 2019 Apr;33(4):203-213.
5. Marx RE. Bone and bone graft healing. Oral MaxillofacSurgClin North Am. 2007 Nov;19(4):455-66.
6. DeLacure MD. Physiology of bone healing and bone grafts. OtolaryngolClin North Am. 1994 Oct;27(5):859-74.
7. Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012 Oct-Dec;8(4):114-24.
8. Goldberg VM, Stevenson S. The biology of bone grafts. SeminArthroplasty. 1993 Apr;4(2):58-63.
9. Kumar P, Vinitha B, Fathima G. Bone grafts in dentistry. J Pharm Bioallied Sci. 2013 Jun;5(Suppl 1):S125-7.
10. Misch CE, Dietsh F. Bone-grafting materials in implant dentistry. Implant Dent. 1993 Fall;2(3):158-67.
11. Elsalanty ME, Genecov DG. Bone grafts in craniofacial surgery. Craniomaxillofac Trauma Reconstr. 2009 Oct;2(3):125-34.
12. Louis PJ, Sittitavornwong S. Managing Bone Grafts for the Mandible. Oral MaxillofacSurgClin North Am. 2019 May;31(2):317-330.
13. Burchardt H. The biology of bone graft repair. ClinOrthopRelat Res. 1983 Apr;(174):28-42.
14. Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am AcadOrthop Surg. 2005 Jan-Feb;13(1):77-86.
15. Perry CR. Bone repair techniques, bone graft, and bone graft substitutes. ClinOrthopRelat Res. 1999 Mar;(360):71-86.
16. Burchardt H. Biology of bone transplantation. OrthopClin North Am. 1987 Apr;18(2):187-96.
17. Pippi R. Post-Surgical Clinical Monitoring of Soft Tissue Wound Healing in Periodontal and Implant Surgery. Int J Med Sci. 2017 Jul 18;14(8):721-728.
18. Mittal Y, Jindal G, Garg S. Bone manipulation procedures in dental implants. Indian J Dent. 2016 Apr-Jun;7(2):86-94.
19. Brugnami F, Caiazzo A, Leone C. Local intraoral autologous bone harvesting for dental implant treatment: alternative sources and criteria of choice. Keio J Med. 2009 Mar;58(1):24-8.
20. Pandit N, Pandit IK. Autogenous bone grafts in periodontal practice: A literature review. J IntClin Dent Res Organ 2016;8:27-33
21. Zouhary KJ. Bone graft harvesting from distant sites: concepts and techniques. Oral MaxillofacSurgClin North Am. 2010 Aug;22(3):301-16.
22. Catone GA, Reimer BL, McNeir D, Ray R. Tibial autogenous cancellous bone as an alternative donor site in maxillofacial surgery: a preliminary report. J Oral Maxillofac Surg. 1992 Dec;50(12):1258-63.
23. O’Keefe RM Jr, Reimer BL, Botterfield SL. Harvesting of autogenous bone graft from the proximal tibial metaphysis. A review of 230 cases. J Orthop Trauma. 1991;5(4):469-474.
24. Moskalewsky S, Osiecka A, Maleczyk J. Comparison of bone formed intramuscularly after transplantation of scapular and calvarial osteoblasts. Bone. 1988;9(2):101-106.

















Comments