Abstract
A variety of surgical procedures can be performed for the treatment of gingival recession, including the subepithelial connective tissue graft. Due to the morbidity reported by patients, alternative techniques using biomaterials has been frequently discussed. The fine gingival biotype tends to be delicate, possessing a small zone of keratinized mucosa and should be taken into special consideration since it directly influences esthetics and emergence profile. The objective of this study was to report the clinical follow-up of root coverage with coronally positioned flap using Mucograft® (collagen matrix) for 12 months. The graft was effective for the thickness of the gingival tissue and can be considered as a viable treatment option for periodontal tissue augmentation. Keywords: Connective tissue graft, esthetics, gingival recession, periodontal grafts

Introduction
In todays era , cosmetic treatment seeks high demand. One of the reasons patient reports to a dental clinic is for receding gingiva and subsequent root coverage procedures.1
Gingival recession is defined as the apical displacement of the gingival margin from the cemento-enamel junction with root exposure, which can be localized or generalized and can include one or more surfaces of the tooth.2
Etiological factors may be associated with,

A variety of surgical procedures may be performed for the treatment of gingival recessions; however, it is necessary to determine the classification of the recession according to Miller,4 and then establish the appropriate surgical treatment and prognosis for each specific case.2

The surgical treatments of root coverage include
- free gingival graft
- subepithelial connective tissue graft with coronal repositioning
- tunnel subepithelial connective tissue graft technique
- coronally positioned flap
- laterally positioned flap
- double papilla technique
- a combination of two or more techniques.5
Root coverage procedures, just like any other, should only be performed if the patient presents healthy gingiva and a good level of oral hygiene.
Favorable results with full coverage are possible in Miller Class I and II recessions. Miller Class III has a dubious prognosis, generally allowing partial coverage of the recession.3 The most predictable treatment, considered the “gold standard” for root coverage, is the subepithelial connective tissue graft. However, this technique offers a disadvantage related to the morbidity to the patient, where it is necessary to remove the connective tissue from the palate area. Adverse effects reported by individuals who have undergone this technique are discomfort and postoperative pain in the palate wound.6
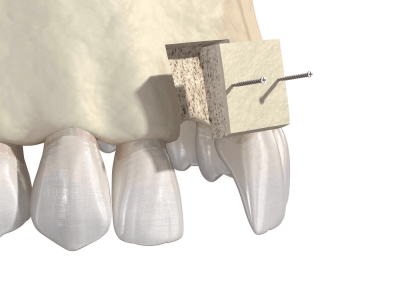
An alternative treatment to eliminate the need for a second surgical area-usually the palate is to use a graft material, such as the porcine collagen matrix. Recently, Geistlich Pharma AG (Wolhusen, Switzerland) produced an absorbable collagen matrix of porcine origin, namely Mucograft®.7 According to Herford et al. (2012), this matrix is indicated for soft tissue augmentation and consists of a bilayer structure:
- A dense layer of compact collagen and
- a spongy layer of porous collagen.8
The objective of this study was to report the clinical followup of root coverage procedure with coronally positioned flap using Mucograft® (collagen matrix) for 12 months.
Case Report
A 35 years old man seek for periodontal treatment due to root exposure in the upper right canine and first molar. At the clinical examination, gingival recessions Miller Class III (Figure 1) was observed. The patient reported no systemic diseases.

Radiographically, there were no suggestive images of caries or periapical alterations.
Initially, the patient was treated with basic periodontal procedures of supragingival scaling and root planing, and oral hygiene instruction were given. The upper right canine tooth to first molar tooth showed 2.5mm to 3mm of gingival recession. The planning included root coverage surgery with a 15 × 20 mm Mucograft® collagen matrix (Geistlich Pharma AG, Wolhusen, Switzerland) associated with coronally positioned flap. After local anesthesia, an intrasulcular incision was performed on the buccal aspect from the upper right central incisor tooth to the distal of the right second molar.
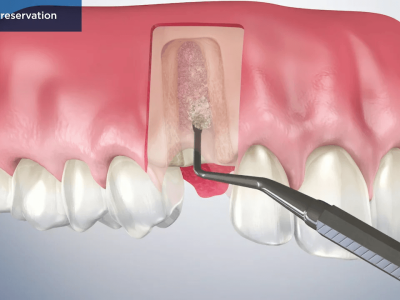
A partial thickness flap was then executed, except on the central and lateral incisors, where a total thickness flap was carried out (Figure 2).

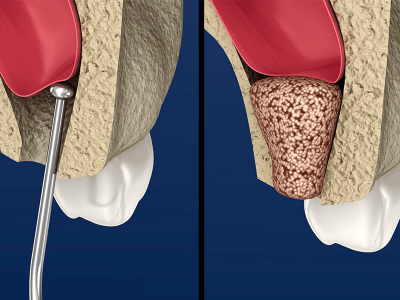
Root planing was performed with Gracey curettes and decontamination of the surfaces was executed using tetracycline hydrochloride and saline solutions for 30 seconds in each root surface. After preparation of the exposed root, the graft was adapted according to the size of each tooth root and positioned following the manufacturer’s instructions (Figure 3).

Two simple sutures were performed to stabilize the graft using Vicryl 6.0 suture material (Ethicon, São Paulo, Brazil). Suspensory sutures in the coronally positioned flap were finally executed (Figure 4).

Post-operative Instructions
Medications:
- Anti-inflammatory (nimesulide 100mg, every 12 h for 5 days),
- Analgesic (Paracetamol 500 mg, every 6 h for 3 days) and
- Antibiotic (Amoxicillin 500 mg, every 8 h for 7 days) were prescribed postoperatively.
Oral hygiene measures:
- Mouthwashe of 0.12% chlorhexidine were prescribed twice a day for 7 days.
- The patient was advised to suspend brushing in the operated area.
Follow-up
The sutures were removed 14 days after surgery (Figure 5).

The measurements were performed after every 6 months.
After 12 months (Figure 6), the results were again measured and satisfactory root coverage was obtained.

Discussion
Several techniques have been presented as treatment for gingival recession, all of them aiming to achieve full coverage of the recession, improve the esthetic condition and decrease sensitivity, while maintaining periodontal health.9
The subepithelial connective tissue graft associated with coronally positioned flap is a technique with high predictability, which has been presenting the best esthetic results among other procedures. However, the morbidity of removing connective tissue from palate is a frailty of this technique; thus, there is an interest in searching for less invasive alternatives, such as the one reported in this case.
To exclude the need for the connective tissue grafts, the Mucograft® was developed; it consists of a xenogenous collagen matrix originated from porcine and composed of collagen Type I and III. It has a bilayer structure, where
- the less porous surface is elastic, ensuring structural integrity of the material and allowing the suture stabilization in the surgical area that receive the matrix; and
- more porous surface that allows adherence, which promotes healing and cell integration.
Thus, as performed in this case, the more porous surface of the collagen matrix contacts the bone defect to facilitate tissue growth and stabilize the clot.
This collagen matrix is specific to regenerate soft tissues and may be used alternatively to increase the volume of keratinized gingiva.7 In the present case, the matrix was used to cover the multiple gingival recessions and increase the tissue thickness. The clinical use of Mucograft® have presented satisfactory clinical results. The results using collagen matrix are similar to the results obtained for subepithelial connective tissue grafts, especially regarding the color.
Conclusion
The root coverage with a coronally positioned flap using Mucograft®, a bilayered collagen matrix for this clinical case was effective. A significant increase in thickness of the gingival tissue that received the collagen matrix was observed; thus, it can be considered a viable treatment option and a suitable graft for soft tissue augmentation.
References
1. Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J Clin Periodontol 2008;35 8 Suppl:136-62.
2. Kassab MM, Badawi H, Dentino AR. Treatment of gingival recession. Dent Clin North Am 2010;54:129-40.
3. Tugnait A, Clerehugh V. Gingival recession-its significance and management. J Dent 2001;29(6):381-94.
4. Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent 1985;5(2):8-13.
5. Dembowska E, Drozdzik A. Subepithelial connective tissue graft in the treatment of multiple gingival recession. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 007;104(3):e1-7.
6. Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession-type defects? J Dent 2008;36(9):659-71.
7. Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M. Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: A randomized prospective clinical trial. J Clin Periodontol 2009;36(10):868-76.
8. Herford AS, Lu M, Akin L, Cicciù M. Evaluation of a porcine matrix with and without platelet-derived growth factor for bone graft coverage in pigs. Int J Oral Maxillofac Implants 2012;27(6):1351-8.
9. Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: A systematic review. J Clin Periodontol 2002;29 Suppl 3:178-94.
10. Rotundo R, Pini-Prato G. Use of a new collagen matrix (mucograft) for the treatment of multiple gingival recessions: Case reports. Int J Periodontics Restorative Dent 2012;32(4):413-9.
Author: Dr Mohini Daultani

















Comments