In a groundbreaking development, a team of researchers led by developmental biologist Michael Levin at Tufts University has successfully created tiny robots made of human cells, known as “anthrobots,” capable of repairing damaged neural tissue. This achievement opens new possibilities for personalized medicine and heralds what some scientists are calling “tissue engineering 2.0.”
The research, published in Advanced Science, represents a significant leap from previous work with “xenobots,” tiny robots made from clumps of embryonic frog cells. Unlike their predecessors, anthrobots are constructed using human tracheal cells and are capable of self-assembly, eliminating the need for manual shaping.
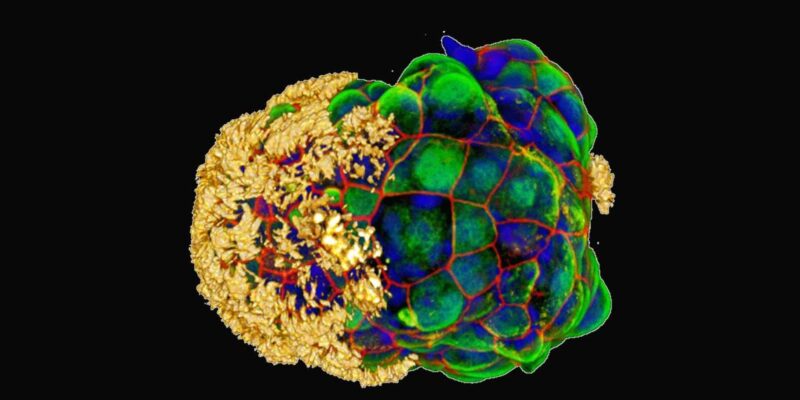
To create these anthrobots, the researchers grew spheroids of human tracheal skin cells in a gel for two weeks. Subsequently, they transferred the clusters to a less viscous solution for an additional week. This caused the tiny hairs on the cells, known as cilia, to move to the outside of the spheroids, enabling them to act as oars. The resulting anthrobots, composed of a few hundred cells each, displayed various swimming patterns, including straight lines, circles, and chaotic movements.
In a remarkable demonstration of their therapeutic potential, the researchers placed several anthrobots in a small dish. The anthrobots autonomously fused to form a ‘superbot,’ which was then placed on a layer of neural tissue that had been intentionally scratched. Astonishingly, within just three days, the sheet of neurons had completely healed under the influence of the super bot.
Study co-author Gizem Gumuskaya, a developmental biologist at Tufts, emphasized the surprising aspect of the research, stating that the anthrobot cells demonstrated their repair function without requiring any genetic modification. This opens the door to potential applications in medical procedures such as clearing arteries, breaking up mucus, and drug delivery, all without the need for genetic engineering.
Looking ahead, Levin and his team believe that anthrobots made from a person’s tissue could be used in regenerative medicine, including limb regrowth. By combining different cell types and exploring various stimuli, the researchers also envision the development of biobots—robots made from biological material—with applications ranging from sustainable construction to outer space exploration.
“Once we understand what cell collectives are willing and able to do, then we can begin to control that not just for stand-alone bots, but for regenerative medicine,” Levin explained. The research hints at a future where the integration of synthetic biology and robotics could revolutionize medical treatments and open doors to unprecedented possibilities in healthcare.
Source : doi: https://doi.org/10.1038/d41586-023-03777-x



















Comments