(This is a part of the ‘Implant Dentistry – Updated Yet Simplified Series’ by prosthodontist & implantologist Dr Nupur Shrirao)
Dental implants are routinely used by clinicians world wide to replace missing tooth/teeth. Research focus on implants over the years, better understanding of body’s responses to implants, and long term follow-ups with various prosthetic options have broadened treatment options. With an increasing number of clinicians providing implant therapy, it is crucial to ensure that the treatment methods used meet global clinical standards.
Once a tooth is indicated for extraction and implant placement, one of the first and most important decision to be made by the clinician is to select an appropriate protocol for implant placement and loading. It is imperative to be familiar with and completely understand these protocols.
Original Protocols of Implant Placement
The original protocols of implant placement required a completely healed alveolar ridge and involved a two stage surgical procedure.
However, with advancements in implant designs and surface coatings, along with a better understanding of bone/implant interface, healing process, occlusion and proper prosthetic design, immediately placed implants gained acceptance.
(Schroeder, 1976 & Branemark,1977)
Understanding The Terms of Implant Placement
Implant placement protocols are defined as follows:
- Immediate implant placement: Dental implants are placed in the socket on the same day as tooth extraction.
- Early implant placement: Dental implants are placed with soft tissue healing (4–8 weeks) or with partial bone healing (12–16 weeks) after tooth extraction.
- Late implant placement: Dental implants are placed after complete bone healing, more than 6 months after tooth extraction.
(Chen & Buser, 2009; Chen et al, 2004; & Hammerle et al, 2009)
Original Protocols of Implant Loading
The original protocols of implant loading required an undisturbed healing time of 3-4 months before loading.
Immediate loading first came into acceptance in fully edentulous sites, where a minimum of 4 implants were placed with cross arch splinting.
However, with research focus on reduction of surgical trauma causing bone necrosis and bone regeneration, along with a better understanding of bone/implant interface, healing process, occlusion and proper prosthetic design, immediately loaded implants gained acceptance in partially edentulous sites as well.
(Schroeder,1976; Adell,1981; Buser, 2000)
(Ledermann, 1979 & Babbush, 1986 researched immediate loading in fully edentulous sites)
Understanding The Terms of Implant Loading
Implant loading protocols were defined as follows:
- Immediate loading: Dental implants are connected to a prosthesis in occlusion with the opposing arch within 1 week subsequent to implant placement i.e. immediate functional loading.
- Immediate restoration: Dental implants are connected to a prosthesis held out of occlusion with the opposing arch within 1 week subsequent to implant placement i.e. immediate non-functional loading.
- Early loading: Dental implants are connected to the prosthesis between 1 week and 2 months after implant placement.
- Conventional loading: Dental implants are allowed a healing period of more than 2 months after implant placement with no connection of the prosthesis.
(Weber et al, 2009 & Gallucci et al,2014)
Current Concepts of Implant Placement & Loading
Current concepts are defined in a ITI consensus 2018 by Gallucci and coworkers.
The terms explained above are assigned a number (for implant placement) and a letter (for implant loading) as follows:
- Type 1 – Immediate Placement
- Type 2 – Early Placement with Soft Tissue Healing
- Type 3 – Early Placement with Partial Bone Healing
- Type 4 – Late Placement
- Type A – Immediate Restoration/Loading (Immediate loading can be a provisional or a final prosthesis)
- Type B – Early Loading
- Type C – Conventional Loading
It is a novel classification combining placement and loading protocols in oral implantology in 12 different combinations as follows:
- Type 1A: Immediate Placement + Immediate Restoration/Loading
- Type 1B: Immediate Placement + Early Loading
- Type 1C: Immediate Placement + Conventional Loading
- Type 2A: Early Placement with Soft Tissue Healing + Immediate Restoration/Loading
- Type 2B: Early placement with Soft Tissue Healing + Early Loading
- Type 2C: Early Placement with Soft Tissue Healing + Conventional Loading
- Type 3A: Early Placement with Partial Bone Healing + Immediate Restoration/Loading
- Type 3B: Early placement with Partial Bone Healing + Early Loading
- Type 3C: Early Placement with Partial Bone Healing + Conventional Loading
- Type 4A: Late Placement + Immediate Restoration/Loading
- Type 4B: Late Placement + Early Loading
- Type 4C: Late Placement + Conventional Loading.
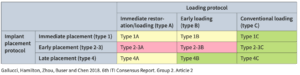
Copyright & Credits – ITI & Quintessence Publications. Color zones explained further in text.
Timeline of Implant Placement & Loading
The timeline is based on the definitions of implant placement and loading protocols (after Zhou & coworkers in 2021).
The terms explained above follow the timeline as follows:
- Type 1 – Immediate Placement – Same Day of Extraction
- Type 2 – Early Placement with Soft Tissue Healing – After 4-8 weeks (1-2 months) of Extraction
- Type 3 – Early Placement with Partial Bone Healing – After 12-16 weeks (3-4 months) of Extraction
- Type 4 – Late Placement – After more than 6 months of Extraction
- Type A – Immediate Restoration/Loading – Within 1 week of Placement
- Type B – Early Loading – After 1 week – 2 months of Placement
- Type C – Conventional Loading – More than 2 months of Placement
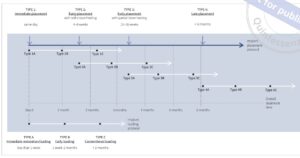
Copyright & Credits – ITI & Quintessence Publications
Evidence Based Implant Protocols
While 12 different combinations are theoretically possible, the practical application of each has to be studied by stringent scouting through available literature, case reports, case series and mass research papers. In a systematic review by German Gallucci et al, 70 papers including randomised controlled trials, clinical trials, prospective and retrospective studies were analysed. On the basis of this evidence, implant placement and loading protocols in partially edentulous sites were scientifically or clinically, documented or validated into three zones as given below.
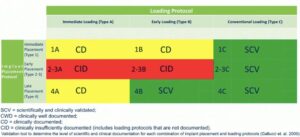
Copyright & Credits – ITI & Wiley Publications
- For Type 1 placement, the loading protocol appears influential in the treatment outcome, with Type 1C being the only approach scientifically and clinically validated.
- For Type 1A, Type B, and Type C, specific placement and loading criteria are required to ensure the clinical efficacy of these treatment modalities.
- Type 2-3C was scientifically and clinically validated and should be considered routine.
- Type 2-3B showed promising results and more evidence is needed to validate this approach.
- Type 2-3A was not reported yet.
In simpler words, for the clinician:
- Green zone: Safest to perform
- Yellow zone: Safe to perform, requires good knowledge & clinical skill
- Red zone: Better to avoid
Clinical Recommendations by ITI
1) Implant placement and loading protocol should be planned prior to tooth extraction
Treatment planning for implant therapy should commence once the indication for tooth extraction has been confirmed. Both the implant placement and loading protocol should be planned prior to tooth extraction. The selection of the implant placement and restoration/loading protocol should be based on achieving predictable outcomes:
- Long-term hard and soft tissue stability
- Optimal esthetics
- Reduced risk for complications
- Meet patient-specific and site-related criteria
2) Alternative treatment modalities should be in place as part of the planning and consent process
As part of the planning and consent process, alternative treatment modalities should be in place, in the event that specific intra-operative procedural criteria are not met. Implant placement and restoration/loading protocols present with different levels of clinical difficulty and overall treatment risk. When selecting treatment modalities, clinician skill and experience should match the challenges associated with the selected protocol.
3)When considering placement and loading protocols, multiple factors can affect intended treatment outcome
When considering placement/loading protocols, there are factors that can prevent the accomplishing of the intended treatment. They must be taken into consideration and discussed with the patient before-hand. These factors include:
- Patient-related factors.
- Lack of primary stability.
- The need for bone augmentation.
4) Patient-centered benefits of the different implant placement, loading protocols and associated risks should be considered
The implant placement and loading protocol can have a negative impact on survival and success of specific selection criteria are not met, and/or execution of the clinical procedure is of insufficient quality. Careful consideration of patient-centered benefits of the different implant placement and loading protocols and the associated risks should be taken into consideration.
5) Type 1A protocol should only be considered when there are patient-centered advantages with good clinical conditions
Immediate placement and immediate restoration/loading (type 1A) is a complex surgical and prosthodontic procedure and should only be performed by clinicians with a high level of clinical skill and experience. Type 1A protocol should only be considered when there are patient-centered advantages (e.g., aesthetic requirements, reduced morbidity), and when the following clinical conditions are met:
- Intact socket walls.
- Facial bone wall at least 1 mm in thickness.
- Thick soft tissue.
- No acute infection at the site.
- The availability of bone apical and lingual to the socket to provide primary stability.
- Insertion torque 25–40 Ncm and/or ISQ value >70.
- An occlusal scheme which allows for protection of the provisional restoration during function.
- Patient compliance.
5) Conventional loading is well documented and recommended with early implant placement
Early implant placement may be considered in most clinical situations, such as sites with thin facial walls and defects, often requiring simultaneous bone augmentation procedures. Conventional loading (type 2-3C) is well documented and is recommended with early implant placement. Immediate (type 2-3A) and early (type 2-3B) loading protocols combined with early implant placement are not sufficiently well documented to be recommended as routine procedures.
6) Late implant placement is the least desirable option due to the risk of alveolar ridge resorption
As a planned procedure, late implant placement is the least desirable of the placement time options, due to the risk of alveolar ridge resorption and reduction in bone volume, as well as extended treatment time. When late placement is indication for patient- or site-related reasons, an alveolar ridge preservation procedure is recommended.
7) Early loading and conventional loading are well-documented protocols for late implant placement
In the case of late implant placement, early loading (type 4B) and conventional loading (type 4C) are well-documented protocols and may be considered routine. Late implant placement with immediate loading (type 4A) may be considered when patient-centered advantages are present, and the criteria for immediate restoration/loading are met.
I hope I could simplify the current protocols of implant placement and loading for you! For any doubts, queries (or positive feedback), drop in your comments below!




















Comments