Dr Shishir Mohan Devki 1, Dr Venkatesh Balaji Hange 2, Dr Hasti Kankariya 3, Dr Shrey Shrivastava 4
1 Head of the Department, Professor 3,2,4 Postgraduate Student
123 Department Of Oral and Maxillofacial Surgery
KD Dental College And Hospital
ABSTRACT: Temporomandibular joint (TMJ) dislocation is a distressing condition characterised by locking of the mandibular condyle anterior to the articular eminence and inability of the patient to close their mouth. Various non-surgical and surgical modalities have been described in the literature with variable success. There is no definite consensus regarding superiority of any treatment modality over the other.
(1) Recently autologus blood transfusion injection has been used to treat recurrent TMJ dislocation. Schulz first described autologous blood injection for treating recurrent TMJ dislocation in 1973. (2)
INTRODUCTION: Dislocation of the TMJ occurs, when the head of the condyle moves anteriorly over the articular eminence into such a position that it cannot be returned voluntarily to its normal position. Luxation of the joint refers to complete dislocation, while subluxation is a partial or incomplete dislocation, actually a form of hypermobility. (1) TMJ dislocation can occur during simple activities such as laughing and yawning; it may occur after excessive mouth opening during dental treatment, tracheal intubation or episodes of vomiting.
There is a higher frequency of TMJ dislocation in patients with Parkinsonʼs Disease or cerebrovascular disorders, which is attributed to masticatory muscle incoordination. A person with TMJ dislocation is unable to close their mouth, which remains locked open until a mechanical reduction is performed. Frequent dislocation episodes characterise a condition referred to as recurrent TMJ dislocation. Thus, patients with this problem risk TMJ dislocation simply by carrying out their daily activities; this disorder can be especially dangerous when self-reduction of the TMJ dislocation is difficult or impossible. (2) Acute mandibular dislocation is usually managed by manually pressing the mandible downwards and then pulling it back upwards in an attempt to try relocating the condyle in the glenoid fossa. If the condyle continues to dislocate several times, it is described as chronic recurrent TMJ dislocation.
Dislocation of TMJ is generally of unknown origin, while several theories have been put forward to explain its onset, it is commonly associated with poor development of the articular fossa, laxity of the temporomandibular ligament or joint capsule and excessive activity of the lateral pterygoid and infrahyoid muscles due to drug use or disease. Additionally some disorders of collagen metabolism such as ligamentous hyperlaxity and Ehler-Danlos syndrome might be related. (3)
Dislocation of TMJ is generally of unknown origin, while several theories have been put forward to explain its onset, it is commonly associated with poor development of the articular fossa, laxity of the temporomandibular ligament or joint capsule and excessive activity of the lateral pterygoid and infrahyoid muscles due to drug use or disease. Additionally some disorders of collagen metabolism such as ligamentous hyperlaxity and Ehler-Danlos syndrome might be related. (3)
The decision depends on predisposing factors and the TMJ morphology. The more complex and invasive methods of treatment might not necessarily offer the best treatment option and outcome; less invasive approaches should be utilised appropriately before adopting the more invasive surgical techniques. Chronic recurrent dislocation may be approached with conservative procedures, including injection of botulinum toxin to various muscles of mastication, injection of sclerosing agents and autologous blood injection into the pericapsular tissue and superior joint space. (4)
Schulz [9] first described autologous blood injection for treating recurrent TMJ dislocation in 1973. In Japan, Takahashi et al. first reported the efficacy of autologous blood injection in a compromised patient who was unable to receive surgery in 2003. The reported overall success rate of autologous blood injection is approximately 80 percent.
Blood injections into the TMJ follow the pathophysiology of bleeding in the joints elsewhere in the body, such as the knee and the elbow. During the first few hours or days, an inflammatory reaction takes place, resulting in the release of inflammatory mediators by platelets along with the accumulation of dead and injured cells, leading to oedema of the joint tissue. This inflammatory reaction diminishes joint mobility. Thereafter, a combination of organised blood clots and loose fibrous tissue forms, which further decreases joint mobility. These tissues mature, causing a permanent limitation of joint movement. This exposure of cartilage to blood results in a disturbance of the cartilage matrix turnover and a decrease in chondrocyte metabolism, causing localised contraction. (4,5)
SURGICAL TECHNIQUE: Patient’s face is prepared. Local anaesthesia (2% lidocaine with 1:100,000 epinephrine) is applied to the auriculotemporal nerve. The articular fossa point (AF) is located at a point 10 mm anterior to the tragus and 2 mm inferior to the tragal-canthal line. At this location, a 19-gauge needle was inserted into the superior joint space of the TMJ; the correct location of the needle is confirmed by movement of the mandible during the fluid injection. Blood is withdrawn (3 ml) from the patient’s anticubital fossa; 2 ml of blood is injected into the superior joint space and 1 ml onto the outer surface of the TMJ capsule. The same procedure is performed on the contralateral TMJ. An elastic bandage is applied around the patient’s head and left in place for the first 24 h.
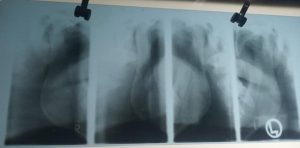
FIG.1 TMJ View Open & Closed Showing Dislocation
CASE REPORT: A 24 year old male patient reported to Department of Oral and Maxillofacial surgery, KD Dental College and Hospital with the chief complaint of recurrent locking of lower jaw and inability to close their mouth. History dates back to approximately 2-3 years, when the patient first experienced this distressing condition. Patient remained stable for variable time followed by recurrence.
Fig.2 OPG Showing Right Recurrent TMJ Dislocation
The condition was managed by manual reduction by various local clinicians. There was

marked deterioration of the condition with multiple episodes of dislocation per day. The diagnosis of TMJ dislocation was based on case history and clinical presentation which later confirmed by radiographic findings. It was decided to perform minimally invasive treatment modality. Restrictions to mouth opening by intermaxillary fixation using Erich’s arch bar seemed appropriate. Patient was informed regarding the procedure and written consent was taken.

Patient was under intermaxillary fixation for 2 weeks and a liquid diet was advised. After 2 weeks IMF was released and patient was followed up with for 2 months
Fig.3. Showing transfusion of Autologus Blood to TMJ
Patient showed relief in the number of occurrence of dislocations but dislocations continued even after restricted mouth opening for 2 weeks.
It was decided to use autologous blood injection therapy as patient was against surgical intervention seems. Patient was informed regarding the procedure and written consent taken. Arthrocentesis followed by injection of autologous blood only in the right TMJ space and adjacent pericapsular tissue as the right TMJ had the most discomfort as compared to contralateral side. Local anaesthesia was administered to block the auriculotemporal nerve.
This was followed by injecting 2 ml of autologous blood into the upper joint space and 1 ml around pericapsular tissue. Injection of blood was followed by opening the mouth and manipulation of the mandible forward to open the joint space.
For the purpose of restriction in mouth opening intermaxillary fixation using ivy eyelet wiring was done for 2 weeks. During post-operative period

FIg.4. Showing Post Operative Mouth Opening
patient experienced significant tightening of right TMJ with reduction in mouth opening. The result of autologous blood injection was highly encouraging in this patient.
DISCUSSION: TMJ dislocation occurs because of variable factors which prevent the condyle from translating back to the condylar fossa. These factors are laxity of the TMJ ligaments,weakness of the TMJ capsule, an unusual eminence size or projection, muscle hyperactivity or spasm, trauma and abnormal chewing movements that do not allow the condyle to translate back. Recurrent TMJ dislocation may cause injury to the disc, the capsule and the ligaments, leading to the TMJ internal derangement. (1)
Methods of treating recurrent TMJ dislocation range from conservative treatment to surgical interventions. Conservative treatments such as restricting mandibular motion with a chin cap, an elastic facial bandage or maxillomandibular fixation often fail to manage the condition. Whereas surgical treatment through eminectomy is considered the gold standard in the treatment of recurrent TMJ dislocation with success rates greater than 85%. multiple surgical interventions were developed including ,capsular placation,temporalis tendon scarification, and lateral pterygoid myotomy may have a high success rate,but it is an invasive procedure requiring general anesthesia, a hospital stay and a skin incision, in addition to increased risk of facial nerve injury. (2)
Non surgical methods are usually first applied to the patients before decision of surgery. There were some successful nonsurgical treatment models described in the literatures such as injection of a sclerosing solution into the joint cavity (tincture of iodine, alcohol and sodium psylliate). However, many side effects and the possible risk of facial paralysis or traumatic arthritis have hindered its widespread usage.Another procedure with less side effects is the use of botox. The toxin temporarily causes denervation of the muscles that draw the chin down. The muscle of choice for injection is the lateral pterygoid muscle. In this way, the displacement of the condyle is prevented even when the mouth is opened excessively. (3)
Autologous blood injection as a treatment of recurrent TMJ dislocation was reported by Brachmann in 1964. He successfully treated 60 patients by autologous blood injections into their TMJ. The therapy is based on the principle to restrict mandibular movements by inducing fibrosis in upper joint space, pericapsular tissues or both. (6)
There are no universally accepted guidelines for this therapy. The protocol differs amongst various clinicians. So, the autohaemotherapy includes the injection of autologous blood only into pericapsular tissues, upper joint space or into both upper joint space and pericapsularly. The volume of blood to be used ranges from 2 ml – 4 ml in the upper joint space and 1.0 – 1.5 ml into pericapsular structures. (7) To further enhance the fibrosis in and around the TMJ a period of restricted mouth opening was advocated in the literature. The protocol for mandibular movement restriction ranges from 7 days – 1 month. (4) The method to restrict mandibular movement utilises conservative elastic bandage head dressing to an aggressive approach of maxillomandibular fixation. (8)
The protocol for repetition of autologous blood injection varies amongst clinicians. Machon et al. advocated that intraarticular injection should be repeated only if there is recurrence of dislocation. Based on their experience, they advocated surgical intervention in case of failure of two intraarticular injections. Few case reports reported successful outcomes even on single blood injections. (9)
Schulz et al repeated pericapsular injection therapy twice a week for 3 weeks. Repetition of injection was not based on the recurrence of attack. Similarly, Khan et al used 3 injections of autologous blood into bilateral TMJ pericapsular tissues spaced at an interval of 5 days each. (10) Critical evaluation of protocols followed by various authors revealed greater success rates in case of use of both intraarticular and pericapsular injections as compared to either intraarticular or pericapsular injections alone. The variable protocols for repetition of injections and mode of mandibular movement restriction, on critical evaluation revealed that the clinicians who used pericapsular injections, advocated frequent repetition irrespective of recurrence. Also, the same clinicians recommended more aggressive form of mandibular restriction in the form of intermaxillary fixation for greater time period of 2 – 4 weeks. (11)
The autologous blood therapy was challenged by some authors who believe that even a brief exposure of the intraarticular cartilage to the blood may lead to decrease chondrocyte metabolism, chondrocyte apoptosis, cartilage degeneration and permanent joint destruction. (12)
Alons et al after inducing haemarthrosis in the TMJ of the rats reported that there is no noticeable damage to the cartilage and interposing disc on histopathological examination. Safran et al in an animal rat model have found that cartilage changes after blood injections were only temporary without any permanent damage. The disadvantage of this technique is the potential for severe restriction in mandibular range of motion. There were some concerns about the procedure such as fibrous or bony ankylosis and articular cartilage degeneration. (1)
There are several advantages of the autohaemotherapy as a treatment modality. As there is no tissue dissection, postoperative complications such as facial nerve injuries, altered sensation, swelling, infection and pain are all decreased or nonexistent. The procedure can be performed in an office setting with or without sedation under local anaesthesia and do not require any sophisticated instrumentation. (4)
Conclusion: Autologous blood injection in the superior joint compartment and around the capsule has been shown to be a safe, simple and cost-effective method for the treatment of chronic recurrent TMJ dislocation. This conservative approach can be tried prior to performance of more invasive surgical intervention. We hope this procedure will prove to be a feasible alternative treatment for patients prior to any surgical intervention.
REFERENCES:
- Autologous blood injection for treatment of recurrent TMJ dislocation: A case report. Gaurav Varma, Sumit Chopra et al., Annals Of Dental Speciality vol.2, issue 27, Jan-Mar 2014, 27-30.
- Autologous blood injection for treatment of recurrent TMJ dislocation. Norie Yoshioka et al., Acta Med. Okayama, 2016, vol 70, no.4, 291-294.
- Autologous blood injection to TMJ: Magnetic resonance imaging findings. Celal Candrili et al., Imaging dentistry science 2012, 42:13-8.
- Arthocentesis followed by intrarticular autologus blood injection for the treatment of recurrent TMJ dislocation. AM Bayomi et al. Int. Journal oral and maxillfac. Surg 2014.
- Srivastava D, Rajadnya M, Chaulhary MK and Srivastava JL: The Dautrey procedure in recurrent dislocation: a review of 12 cases. Int J Oral Maxillofac Surg (1994) 23: 229-231.
- Martinez-Perez D, Garcia Ruiz-Espiga P. Recurrent TMJ dislocation treated with botulinum toxin: Report of 3 cases. J OralMaxillofacial Surg. 2004; 62(2):244-6
- Aquilina P, Vickers R, McKellar G. Reduction of a chronic bilateral TMJ dislocation with intermaxillary fixation and botulinum toxin A. Br J Oral Maxillofac Surg. 2004; 42(3):272-3.
- Qiu WL, Ha Q, Hu QG. Treatment of habitual dislocation of the TMJ with subsynovial injection of sclerosant through arthroscope. Proc Chin Acad Med Sci Peking Union Med Coll. 1989; 4(4):196-9.
- Myrhaug H. A new method of operation for habitual dislocation of the mandible: review of former methods of treatment. Acta Odontol. 1951; 9(3-4):247-60.
- Daif ET. Autologous blood injection as a new treatment modality for chronic recurrent TMJ dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109(1):31-6.
- Schulz S evaluation of periarticular auto-transfusion for therapy of recurrent dislocations of the TMJ. Dtsch Stomatol 1973; 23:94–8.
12. Aurora JK, Singh G, Kumar D, Kumar R, Singh K. Autologous injection for the treatment of recurrent TMJ dislocation – a case report. J Indian Dent Assoc 2011; 5:846–8.



















Will this article available in pdf format?
We will mail you the PDF doc.
Mail the pdf file on venkateshhange@yahoo.com