Abstract
Bone defects of the jaws are frequently ascribed to accidents, congenital anomalies, tooth abscesses, jaw atrophy with ageing, or general disease are frequently implicated in bone deformities of the jaws. Although less known, endodontic surgery uses bone grafting materials more and more frequently these days for bone defects due to large periapical lesions. Bone grafting and guided tissue regeneration are two modern methods that have been developed to treat certain bone abnormalities. This article reviews the most common graft materials and regenerative materials used in endodontics and explain the outcomes of these grafts.

Introduction
Numerous studies in the past have demonstrated a better outcome with regards to tissue healing following periapical surgery with the aid of regenerative technique using bone graft compared to the same lesions without regenerative techniques.(1) The concept of regenerative therapy entails utilization of periosteal grafts with the potential to stimulate bone formation. It allows cellular regrowth of defects caused by pathosis or surgical trauma and has resulted in development of grafts, membrane or barrier. (2) Bone graft may maintain space for new bone formation, provide vital osteogenic cells (osteogenic effect), induce host cells to reconstruct lost bone (osteoinductive effect) and act as scaffolds on which host osteogenic cells might grow (osteoconductive effect) (3)
Bone grafting materials are classified as autograft (derived from same individual), allograft (derived from a different individual from the same species), xenograft (derived from a different species) and alloplasts (derived from synthetic sources). (4)
Autograft: Autografts are obtained from the host and are the gold standard bone replacement grafts because they are osteogenic and induce minimal immune responses.(3)
Allograft: Allograft is is harvested from an individual other than the one receiving the graft.There are three types of bone allograft available. (5)
- Fresh or Fresh frozen bone
- FDBA
- DFDBA
Xenograft: Xenografts are derived from bovine, porcine and coral sources. (4) Alloplastic grafts: Alloplastic grafts may be made from hydroxyapetite,a natural occurring mineral, made from bioactive glass.(5) Some synthetic bonegraft are made of calcium carbonate.(5)The most commonly used bone grafting materials in endodontic surgery are calcium phosphate, hydroxyapatite and demineralized, freeze-dried bone allograft (DFDBA) material. (3)
This article briefly describes different graft materials which are used in Endodontics.
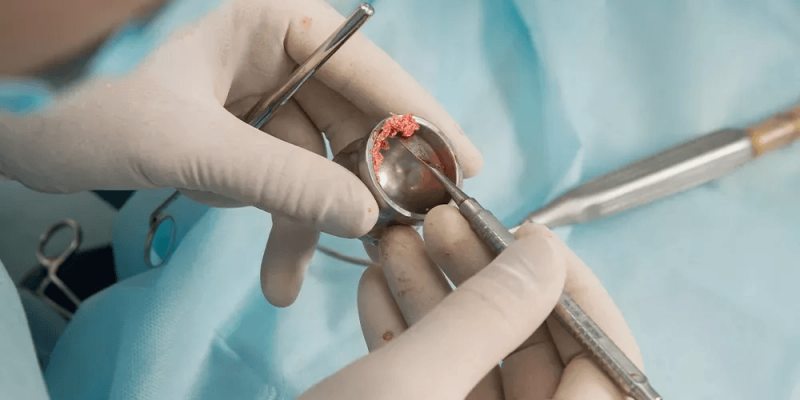
Bone grafts used in Endodontics
Autograft: Due to their osteogenic qualities, autografts are regarded as the “best quality level” among the several available unifying materials. Since a number of developmental factors contribute to the separation of mesenchymal undifferentiated cells into osteoblasts, reasonable cells from the benefactor to the beneficiary site as well as osteoinductive characteristics are also desirable. The risk of an impervious response is zero, with a success rate of >95% because they share the same natural birthplace as the existing life form desirable.
Allograft: Allografts are typically obtained from human cadavers and require to be processed before being used. (4) The most commonly used forms of allograft are freeze-dried bone allograft and decalcified freeze-dried bone allograft (DFDBA). (7) FDBA has osteoconductive potential only whereas DFDBA has both osteoconductive and osteoinductive properties. (8)
Endodontic regeneration has been demonstrated with both FDBA and DFDBA. When used in periapical defects after root end surgery, one endodontic study demonstrated that FDBA results in histological regeneration with no adverse reaction. Many studies showed that healing and new bone formation with FDBA is more rapid. (7)
Alloplastic material: A heterogeneous group of materials including calcium phosphate, calcium sulphate, calcium carbonate, bioactive glasses and polymers is represented in this category. (8) Alloplastic bone substitutes are available in a wide range of sizes and shapes for use in bone replacement or soft tissue support applications. These biomimetic materials aim to act as a three-dimensional framework for bone growth and arrangement, increasing cell adhesion and expansion, without osteoinductive, osteogenetor, or osteogenic components. (6)
Hydroxyapatite is found to be very effective alloplastic material in large bone destruction caused by periradicular lesion. Hydroxyapatite offers the potential of an unlimited supply of bone substance, absence of donor site morbidity, and decreased operative time. Hydroxyapatite is biocompatible, not immunogenic nor antigenic.
Xenograft: Xenografts are bone grafts from a species other than human, such as bovine, calcified matrix is used. (5) They usually possess osteoconductive features with limited resorptive.The disadvantages are the difference in bone characteristic as compared to humans, their processing procedure might affect their physic-chemical properties as in case of allografts, the possibility of disease transmission and stimulation of immunogenicity. (8), (9)
Positive clinical results have been reported for xenografts in the treatment of infrabony, furcation and endodontic related surgical defects. (7).
Two illustration of xenograft used in dentistry are:-
- Bovine substitute: The first xenografts used on patients were bovine-derived bone substitutes, which are among the well-documented materials in this category and are commercially available in a wide range of products. They are osteoconductive, deproteinized, and lyophilized without triggering an immune response.(8)
- Coral substitute: Coral bone grafts have been also applied in jaw defects, exhibiting osteoconductive properties and functioning as carriers for growth factors, improving bone formation.(9)
Limitations of endodontic bone grafts
Inspite of advancements in the field of dentistry, treatment of endodontically involved teeth with large periapical defect still remains a daunting task for a dental surgeon. (2) Periapical apical lesions that are small in size may heal satisfactorily with the aid of resident osteoblast, periodontal ligament cells, and cementoblasts. However, lesions which are too large would require recruitment of stem cells and their differentiation into osteoblast, cementoblast and periodontal ligament cells. (9) This means that the size of the periapical lesion is a big prognostic factor. Delayed healing is seen for the apical lesions >5 mm in diameter.
Regeneration – an alternative to endodontic bone grafts
There are materials that are recently reported with better regeneration than graft repair in endodontic surgeries. They are:
- e-PTFE (non-resorbable expanded polytetrafluoroethylene)
- Bio-absorbable collagen
- Activated Protein C (APC)
These work by preventing the migration of the cells apically and promoting the regeneration.(10)
e-PTFE membranes is one the first materials that is biocompatible used in the endodontic regenerative procedures for the apicectomy. This membrane however is prone to lodging the bacteria that may hamper the outcome in the regenerative procedures for the apicectomy. The recently developed high-density PTFE membrane may overcome this problem.
Collagen membrane works better when combined with bovine derived hydroxyapatite (Bio-GideTM and Bio-OssTM). Itis easily accepted and does not elicit any host response. This precludes the necessity of the second intervention. However, the resorption of the material is slow.
APCs have been increasingly used in the recent as innovative regenerative materials in apicectomy. They have growth factors such as vascular endothelial growth factor, platelet-derived growth factor, and TGF-β. They are extensively used in periodontal surgery; however, their application in apicectomy and other endodontic surgeries has been assessed in only 3 studies as of now. Although the clinical/radiographic results were satisfactory, more clinical studies are warranted to better understand the outcome with these materials.(10)
Conclusion
In the past few decades, a great deal of work has been done in the field of bone graft materials to enhance their properties, such as mechanical strength, biocompatibility and degradation capability in order to closely mimic those of genuine bone. The goal of this article was to make the fundamentals of these materials in endodontics clearer and simpler. To provide each patient with the greatest clinical outcome possible, the practitioner must be aware of these substitutes and properties.
References
- Mirza M. The Rationale for the application of bone grafts in Periapical surgery: A Review. Int J Cur Res Rev. 2021;13(02): 9-12
- Chaturvedy V, Chaturvedy S. Regerative Therapy as an adjunct to Periapical Surgery: A Case Report. Int J Clin Pediatr Dent 2012; 5(1): 75-77
- Liu TJ, Zhou JN &Guo LH. Impact of different regenerative technique and materials on the healing outcome of endodontic surgery: a systemic review meta- analysis International Endodontic Journal 54,536 -555,2021
- Pellegrini GG, Mattiuzzi AS, Pellegrini MA et al. Update on Bone Grafting Material used in dentistry in the bone healing process: Our Experience from translational studies to their clinical use. Bone- Grafting- Recent Advances with special references to craniotomy facial surgery. Intchopen 2018
- Kumar P, Vinitha B & Fathima G. Bone grafts in dentistry. J Pharm Bioallied Sci. 2013 Jun; 5(Suppl 1): S125- S127
- Hassan AH & Bhateja S. Grafts in dentistry– A review. IP Journal of Otorhinolaryngology and Allied Science, October-December 2019;2(4): 90-94
- Bashutski JD, MS, and Wang HL, PHD. Periodontal and Endodontic Regeneration.JOE 2009;35 (3):321-328
- Titsinides S, Agrogiannis G, and Karatzas T. Bone grafting materials in dentoalveolar reconstruction: A comprehensive review. Jpn Dent Sci Rev. 2019 Nov; 55(1): 26-32
- Udayshankar V, R VK, Prakash P, and Jain V.Bone grafts mayerials used in dental Implant: A review. IP Annals of Prosthodontics and Restorative Dentistry, July-September, 2019;5(3):58-62
- Sumangali A, Tiwari RVC, Kollipara J, Mirza MB, Brar RS, Dhewale AM. Various Assisted Bone Regeneration in Apicectomy Defects Systematic Review and Meta Analysis. J Pharm Bioallied Sci. 2021 Nov;13(Suppl 2):S927-S932.



















Comments