Abstract
The multifaceted clinical representation of temporomandibular disorders (TMDs) makes it difficult for clinician to provide a specific treatment plan for patients . A multimodal approach for treatment works best for their management. This article focuses on the manual physiotherapy technique and exercises suggested for management of TMD symptoms. Key words: TMJ,TMD, , Facial pain, Masticatory muscle pain, physical therapy ,manual therapy.
Physical therapy represents a group of conservative supportive activities usually instituted in conjunction or alone with definitive treatment for management of temporomandibular disorders (TMD) symptoms. Physical therapy has two general categories:
- Manual techniques and
- Physical Therapy Modalities.
This article on the manual techniques provides an insight on how a dentist can educate the patient and prescribe exercises for management of TMD.
Manual techniques are exercises provided by the physical therapist or educated to the patient as at-home exercises for the reduction of pain and dysfunction. Manual techniques are divided into three categories:
- Soft tissue mobilization
- Joint mobilization
- Muscle conditioning.
Soft Tissue Mobilization
Soft tissue mobilization is useful for myofascial pain conditions and is achieved by superficial and deep massage which help in regaining normal function and mobility of injured or painful tissues. Manual massages acts as mild stimulation of cutaneous sensory nerves reducing pain perception .
The patient is involve in the treatment process and can be educated to perform self-massage along with painless techniques for stretching of muscles for pain reduction. (Fig 1)
Deep massages are more effective when administered by a physical therapist who may use moist heat for 10-15 min before the initiation of massage therapy , aiding in pain reduction.
Fig 1. The patient is encouraged to apply gentle massage to the painful areas regularly throughout the day
TM Joint Mobilization
Gentle distraction of the TM joint can assist in reducing intraarticular pressure and increase range of motion of joint by reducing temporary adhesions and perhaps even mobilize the disc. Joint distraction have shown help in cases of the acute disc dislocation without reduction.
Painless distraction of the TMJ in absence of inflammation is accomplished by placing the thumb in the patient’s mouth over the lower second molar area on the side to be distracted. With the cranium stabilized by the other hand, the thumb places downward force on the molar as the rest of the same hand pulls up on the anterior portion of the mandible (chin) .Distraction for relaxing muscles does not require translation of the joint, but merely unloading in the closed joint position for several seconds and repeated couple of times. (Fig 2)
Fig 2 TM Joint Distraction of the Temporomandibular Joint. This can be accomplished by placing the thumb in the patient’s mouth over the mandibular second molar area on the side to be distracted. While the cranium is stabilized with the other hand, the thumb exerts downward force on the molar.

Muscle Conditioning
Patient showing signs of TMDs often have prolonged disuse atrophy or shortening of masticatory muscles due to pain. There are four types of self-administered exercise programs that can be instructed to the patient which can help restore the normal function of these muscles.
- Passive muscle stretching
- Assisted muscle stretching
- Resistance exercises
- Postural training.
Passive Muscle Stretching
Gentle passive stretching of a muscle can assist in re-establishing normal muscle length and function. Muscle stretching counteracts the shortened muscle length which contributes to decreased blood flow and the accumulation of algogenic substances that may be responsible for muscle pain.
The patient should be instructed to deliberately open the mouth in comfortable manner until painless range of motion without deviation or protrusive movements (Fig 3). Some patients may show habitual deviation in mouth openings developed due to muscle engrams care should be taken not to overdo the stretching as this may result in aggravating the symptoms.

Fig 3. Passive Exercises – The patient is encouraged to open on a straight opening pathway.
Assisted Muscle Stretching
Assisted muscle stretching helps in myofascial pain by regaining muscle length. Patient should be advised to perform controlled unforceful stretching on their own with fingers and avoid trauma by overstretching. (Fig 4)
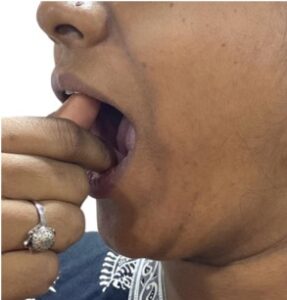
Fig 4. The patient is instructed to apply stretching force gently and intermittently to the elevator muscle with the fingers to assist mouth opening painlessly.
In therapist assisted stretching Spray and stretch technique vapocoolant spray is utilised as a counterirritant before stretching the muscle for eliminating of trigger points. Vapocoolant spray provides a temporary anaesthesia effect to the muscles so that a more intense stretch can be achieved without pain, to be repeated multiple times a day (Fig 5,6). Elimination of trigger points by active stretching of muscles can assure higher treatment success

Fig 5 Spray-and-stretch technique. Vapocoolant spray is applied to the upper trapezius and to the cervical muscles to eliminate myofascial trigger points. The eyes, nose, mouth, and ears are protected from the spray.

Fig 6 Immediately following the spray, the muscles are painlessly stretched by the therapist.
Resistance Exercises
Resistance exercises utilize the concept of reflex relaxation or reciprocal inhibition. When the patient attempts to open, the mandibular depressors are active and elevator muscles, which normally relax slowly, keep the mandible from dropping suddenly. If the depressor muscles meet resistance, the neurologic message sent to the antagonistic muscles (the elevators) is to relax more fully.
Patient should be instructed to perform the following resistance exercises 6-10 times each session, six sessions a day. If they elicit pain, they may be discontinued.
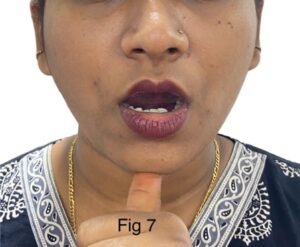
1) The patient is instructed to open against gentle resistance provided by the fingers. This will promote relaxation in the elevator muscles, thus allowing increased mandibular opening. (Fig 7)
2) Ask the patient to restrict eccentric movements, by moving the mandible in an eccentric position against slight resistance with thumb. (Fig 8)

3) Ask the patient to keep tongue on the palate. Place one finger on each TMJ . Allow the lower jaw to partially drop down and back to bring the chin to the throat. Monitor this partial jaw opening in a mirror to make sure the mouth opening is straight. (Fig 9)

4) Ask the patient to keep tongue on the palate. Place one index finger on the TMJ. Place other index finger on chin. Allow the lower jaw to fully drop down and back with help from the index finger. Monitor this full range of motion is straight (tongue stays up). (Fig 10)

5) Patient is asked to bite on to a finger or marker pen with anterior teeth and move jaw from right to left slowly without opening the mouth 10 to 15 times. (Fig 11)
Postural Training
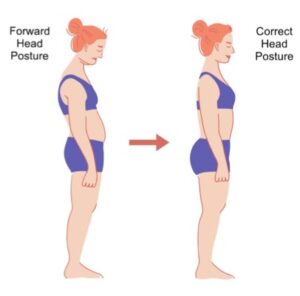
The referred pain pattern caused by central excitation and convergence phenomenon of cranial and cervical nerves are considered major contributors for relationship between the posture of the head, neck, and shoulders and TMD symptoms. Posture in simple terms can be referred as the position of the human body as it is displayed in space. In patients with TMD, the position of the head is depressed as the masticatory muscles change the position of the jaw.
If the head is in the forward position, the patient has to rotate the head upward in order to see adequately, resulting in elongation of the supra and infrahyoid muscles and also closing the posterior space between atlas and axis. Training the patient through exercises to keep the head in a more normal relationship with the shoulders may be helpful in reducing TMD symptoms.
Conclusion
Manual physical techniques should be considered as first line of treatment in management of TMD since these exercises are simple, cost effective , non-invasive and have favourable prognosis.
References
- Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 7. St Louis: Elsevier/Mosby,2013.
- Carlson CR, Okeson JP, Falace DA, et al.: Comparison of psycholog- ical and physiological functioning between patients with masticatory muscle pain andmatched controls, J Orofacial Pain 7:15–22, 1993.
- Magnusson T, Syren M: Therapeutic jaw exercises and interocclusal appliance therapy. A comparison between two common treatments of temporomandibular disorders, Swed Dent J 23(1):27–37, 1999.
- Feine JS, Lund JP: An assessment of the efficacy of physical therapy and physical modalities for the control of chronic musculoskeletal pain, Pain 71(1):5–23, 1997.
- Feine JS, Widmer CG, Lund JP: Physical therapy: a critique (see comments), Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83(1):123–127, 1997.
- Wessberg GA, Carroll WL, Dinham R, Wolford LM: Trans- cutaneous electrical stimulation as an adjunct in the manage- ment of myofascial pain-dysfunction syndrome, J Prosthet Dent 45(3):307–314, 1981.
- Melzack R, Wall PD: Pain mechanisms: a new theory, Science 150:971–979, 1965.
- Clark GT, Green EM, Dornan MR, Flack VF. Craniocervical dysfunction levels in a patient sample from a temporomandibular joint clinic. J Am Dent Assoc 1987;115:251–256.
- Darlow LA, Pesco J, Greenberg MS. The relationship of posture to myofascial pain dysfunction syndrome. J Am Dent Assoc 1987;114:73–75.
- Munhoz WC, Marques AP, de Siqueira JT. Evaluation of body posture in individuals with internaltemporomandibular joint derangement. Cranio 2005;23:269–277.

















Comments