Abstract
A minimally invasive technique, osseodensification, can be used to facilitate maxillary sinus bone graft augmentation for placement of dental implants. The crestal approach is traditionally used in clinical situations where the residual bone height (RBH) under the sinus is greater than 5.0 mm. Implant placement is usually delayed in cases where the RBH is less than 5 mm 1. It has been recently shown that with cautious planning as well as advanced skill and training of the surgeon, this technique may be used in cases where the RBH < 1.5 mm, and can produce a vertical height of augmentation greater than 10 mm 2.
Introduction
Dental implants are the ideal treatment option to replace non-restorable or missing teeth in patients. The placement and restoration of dental implants requires a thorough understanding of treatment planning, surgical and restorative skills, and hygiene maintenance.
When assessing a potential future implant site, if the implant does not “fit” due to a deficiency of hard or soft tissue, then the clinician and patient must commit to a bone graft, tissue graft, or sinus graft to augment that site. The posterior maxilla poses several challenges for the placement of dental implants, like:
- bone and tissue loss from periodontal disease
- post-extraction bone atrophy in both height and width
- pneumatization of the maxillary sinuses
- poor bone density and
- very high occlusal forces.
Bone grafting in the maxillary sinus is the solution to obtain adequate bone volume for implant placement 2.
Numerous successful surgical techniques have been used for indirect sinus augmentation. Some surgical procedures include:
- osteotomes 3
- balloons 4
- reamers 5
- hydraulic pressure 6 and
- osseodensification burs.
The use of osseodensification burs (Densah™) for crestal sinus lift is a safe and effective technique. However the safety and effectiveness of this procedure depends on cautious planning as well as the skill and advanced training of the surgeon 2.
This case report presents the placement of a dental implant in position #27 using osseodensification for the osteotomy preparation as well as for Versah sinus graft protocol I.
Case Report
Tooth #27 had a hopeless prognosis due to severe decay in the furcation and a very large abscess. There was a very large fenestration defect in the buccal cortical plate of bone. The tooth was extracted and mineral cortical allograft was used to graft the socket and augment the buccal ridge.

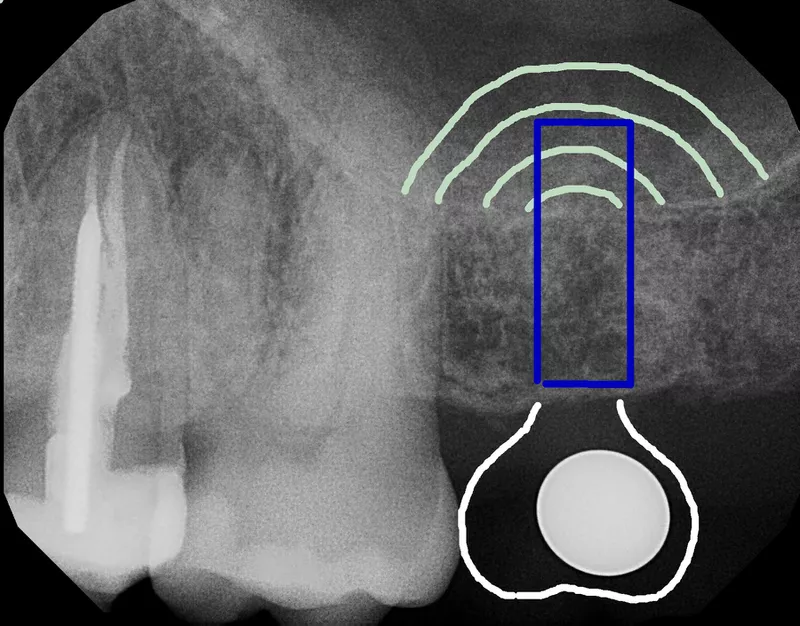
The pre-op x-ray of the implant site in the upper left showed a residual bone height (RBH) of 6.5 mm at position # 27. Tooth # 27 was planned to be replaced with an implant (Astra EV 5.4 S x 11 mm). The implant was planned to be placed subcrestal i.e 4.0 mm below the CEJ of the adjacent tooth. (Fig 1)
A drawing on the pre-op x-ray of tooth # 27 was used to illustrate and plan for the implant & implant crown. A simple drawing such as this allowed pre-surgical 3D orientation of the implant in the bone. The depth of the implant and the emergence profile of the crown can also be planned in this way. (Fig 1)

Careful implant planning was done using a CBCT. The pre-op CBCT of the implant site showed new regenerated bone where there originally was a very large fenestration defect. The CBCT showed a RBH of 6.5 mm to the sinus floor. (Fig 2)

Pre-op occlusal view of the ridge showed a thick ridge of bone with good keratinized tissue on the buccal aspect of the implant site. (Fig 3)

Occlusal view of the ridge on raising the flap showed a thick ridge of bone. (Fig 4)
Osseodensification

The Versah drilling sequence in osseodensifying mode 1100 RPM counter clockwise (CCW) was as follows:
- Pilot drill 1.6 mm
- 2.0 mm
- 2.5 mm
- 3.0 mm
- 3.5 mm
- 4.0 mm
- 4.5 mm
- 5.0 mm.
Copious irrigation with sterile saline was used at every step.
The initial Versah Densah drill (2.0 mm) was advanced only to a depth of 5.5 mm corresponding to 1 mm below the sinus floor. A radiograph was used to confirm this depth.

A radiograph was taken to confirm the initial osteotomy depth is upto 1 mm below the sinus floor. (Fig 6)
The Versah burs were advanced in 1 mm increments just past the sinus floor. The burs are never to be advanced past 3 mm beyond the floor of the sinus.

The guide pin placed in position # 27 was also used to show proper 3D angulation for implant placement. This allowed for confirmation of parallelism & angulation, and proper distance & orientation in both MD and BL directions. The screw access hole was placed in the center of the tooth. The osteotomy was perfectly centered between the teeth in 3 dimensions. (Fig 7)

The final osteotomy bur diameter was 5.0 mm for the placement of a 5.4 mm implant.(Fig 8)

The osseodensified ring of bone (Fig 9). Bone was compacted and auto-grafted outwardly. A strong and dense layer of bone was formed along the walls and base of the osteotomy. The sinus membrane was seen along with a small amount of autogenous bone.
Crestal sinus grafting


The osteotomy was filled with a well hydrated mineralized cancellous allograft (Fig 10,11).

The Densah bur 5.0 was used in osseodensification mode up to 3 mm past the sinus floor at 150 RPM with no irrigation, to propel 0.5 cc mineralized cancellous allograft under the sinus membrane.(Fig 12) This was done very carefully several times. A significant amount of bone was grafted into the maxillary sinus under the membrane.

Radiograph showed the Densah sinus grafting of autogenous bone and mineralized cancellous allograft bone. Note the large dome-shaped grafting of bone in the sinus indicating containment of the bone graft under an intact sinus membrane. (Fig 13)
Position # 27 had a 6.5 mm residual bone height to the sinus floor. Versah sinus grafting produced an increase in bone height of approximately 7 mm for a total bone height of 13 mm.

The Astra EV 5.4S x 11 mm implant was ready for placement in position # 27.(Fig 14) The implant was placed subcrestally 4.0 mm below the CEJ of the adjacent teeth. There was a 2.5 mm thickness of bone on the buccal surface of the implant.

Occlusal view of the implant in place. (Fig 15)

Penguin (Citagenix ™) MulTiPeg was used for implant stability quotient (ISQ) measurement. (Fig 16) Since the primary stability was 52, it was not immediately loaded. The implant was buried with a cover screw to allow healing & integration.

Tension free primary closure was achieved with 5:0 nylon sutures. After integration, an apically repositioned flap was done to cover the implant and augment the amount of keratinized tissue. (Fig 17)

Final radiograph showed the Densah sinus grafting of autogenous bone and mineralized cancellous allograft bone after implant placement and closure. There was an initial RBH of 6.5 mm to the sinus floor. Versah sinus grafting produced an increase in bone height of approximately 7 mm, resulting in total bone height of 13 mm. Note the large dome-shaped grafting of bone in the sinus indicating containment of the bone graft under an intact sinus membrane. (Fig 18)
Healing of the implant surgery was rapid and uneventful with no instance of sinus membrane perforation or other complications seen.
The implant was uncovered after 4 months of healing and integration. The implant now had an ISQ of 89, showing very high stability and was ready to be loaded.


A screwmentable Lava porcelain crown on gold titanium Atlantis custom abutment was used to replace tooth # 27. (Fig 19, 20)

Final radiograph post prosthesis.(Fig 21)
Discussion
Multiple factors are involved in the successful placement of dental implants. Careful treatment planning, surgical skill, well designed prosthetics, and excellent patient maintenance are required. The posterior maxilla frequently poses numerous complications that must be evaluated and overcome prior to dental implant surgery. Poor bone quality and the presence of the maxillary sinus are the main challenges.
The crestal sinus floor elevation is an adjunctive surgical procedure that is often required. Crestal sinus lifts are generally indicated when the residual bone height under the sinus is greater than 5 mm. Osseodensification burs have been shown to be a safe and minimally invasive technique to achieve this result.
Osseodensification – Osseodensification does not create the tissue. It optimizes the bone that is already present.Osseodensifying burs induce a pressure wave ahead of the bur to facilitate the autografting of bone particles along the inner surface walls and apex of the osteotomy. The burs are used to densify the osteotomy, and autocompact bone by pushing autogenous bone apically and outward toward the osteotomy walls. The slurry of irrigation fluid and autogenous bone chips creates the gentle hydraulic detachment and elevation of the Schneiderian membrane 7. The sinus is therefore augmented with a potentially low risk of perforation. Additionally, in this case, the burs were advanced in 1 mm increments just past the sinus floor. The burs are never to be advanced past 3 mm beyond the floor of the sinus.
The ISQ (Implant Stability Quotient) measures the degree of osseointegration and implant stability. A value above 70 means the implant is stable and ready for loading. The implant here had an ISQ of 52 at placement, therefore its primary stability was insufficient to load immediately. At 2nd stage after 4 months of healing, the implant had an ISQ of 89, showing very high stability and hence was loaded with a prosthesis.
Conclusion
The use of dental implants allows patients to regain their lost function, form and esthetics. This case report illustrates the use osseodensification burs for implant osteotomy as well as indirect sinus bone augmentation.
References
- Fugazotto PA. Augmentation of the posterior maxilla: A proposed hierarchy of treatment selection. J Periodontol. 2003;74:1682-1691
- Salgar, N. Osseodensified Crestal Sinus Window Augmentation: An Alternative Procedure to the Lateral Window Technique. J Oral Implantol (2021) 47 (1): 45–55.
- Toffler M. Osteotome-mediated sinus floor elevation: A clinical report. Int J Oral Maxillofac Implants. 2004;19:266-273
- Mazor Z, Kfir E, Lorean A, et al. Flapless approach to maxillary sinus augmentation using minimally invasive antral membrane balloon elevation. Implant Dent. 2011 Dec; 20(6):434-8.
- Ahn SH, Park EJ, Kim ES. Reamer-mediated transalveolar sinus floor elevation without osteotome and simultaneous implant placement in the maxillary molar area: clinical outcomes of 391 implants in 380 patients. Clin Oral Implants Res. 2012 Jul;23(7):866-72.
- Kim JM, Sohn DS, Heo JU et al. Minimally invasive sinus augmentation using ultrasonic piezoelectric vibration and hydraulic pressure: a multicenter retrospective study. Implant Dent. 2012 Dec;21(6):536-42
- Huwais S, Mazor Z, Ioannou AL. A Multicenter Retrospective Clinical Study with Up-to-5-Year Follow-up Utilizing a Method that Enhances Bone Density and Allows for Transcrestal Sinus Augmentation Through Compaction Grafting. Int. J Oral Maxillofac Implants2018;33:1305-1311



















Comments