(This is a part of the ‘Implant Dentistry– Updated Yet Simplified Series’ by prosthodontist & implantologist Dr Nupur Shrirao)
Flap designs in implantology are tailored incisions that expose the surgical site for implant placement, with key considerations including the need for bone grafts, the number of implants, and anatomical structures. Common designs include the trapezoidal and triangular flap, which provide access and allow for tension-free closure. Flapless surgery is an option for simpler cases, while procedures like guided surgery may use soft tissue punches. This article delves into the essentials of incision placements and flap designs, emphasizing its importance in ensuring optimal surgical outcomes.
One of the primary steps in implant placement, is placing an incision for raising an adequate flap. Flap designing serves as an important step both in first and second stage implant surgery. The choice of flap design is crucial for ensuring proper blood supply, adequate visibility, and a successful, well-healed outcome.
The Importance of Incision
Surgical incisions are fundamental to the success of any operative procedure, serving as the gateway to access underlying tissues and organs. A well-chosen surgical incision provides optimal access to the surgical field while minimizing risks and protecting neurovascular structures. The choice of incision, placement, and the technique used are critical factors influencing immediate and long-term outcomes, including patient recovery, morbidity, and cosmetic results.
Tips for Incision Placement
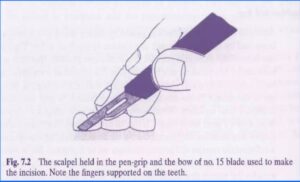
Usually a no 15, 15 C or no 12 blades are used for implant surgeries. Here are some personal tips for placing good incisions:
- Always use a sharp blade. The blade may dull at a faster rate if the resistance of the tissues being cut is more or the incising length is more, like in full arch cases. If the blade does not seem to be incising easily, change the blade and use a fresh one.
- Hold the blade properly. In implantology, since we raise a full thickness flap, the blade must be in continuous contact with the bone. Holding the blade perpendicular to the tissues makes it easier to approximate them during primary closure.
- Give a neat incision by using a firm, continuous stroke. Repeated, tentative strokes increase damaged tissue and bleeding. Pen grip with appropriate finger rest helps in a firmer grip. Do not lift the blade till the incision is complete. Long continuous strokes are preferred to short, interrupted ones.
- Incise in correct tissue – Place incisions in keratinised attached gingiva. If inadequate, place a para median incision rather than a median one. Take care to not place the incision on micro-anatomical structures. Preserve the interdental papilla by placing incisions mesial to it and not through it.
The Importance of Flap Design
Flap design is critical for providing visibility and access to surgical sites. Properly designed flaps allow identification of vital anatomical structures like the mental foramen, incisive canal, and adjacent tooth roots. The primary goal is to maintain the blood supply to the flap, ensuring healthy healing and minimizing complications such as necrosis or scarring.
Principles of Flap designing for Dental Implants
Let us simplify the principles of flap designing taking four considerations into account:
- Flap Raising & Handling
- Flap Repositioning
- Flap Closure
- Special considerations for implants
Flap Raising & Handling: A flap must be designed in such a way that when it is raised, the blood supply to the flap is preserved, and that the soft tissue of the implant site and of the adjacent teeth are not damaged. Vertical incisions if given, should be oblique to ensure broad base of flap. A full thickness mucoperiosteal flap is raised for implant surgeries. It must be raised with care.
Do not play with the flap! Careful flap handling means that the flap should not be excessively twisted, stretched or grasped since this may damage the blood vessels supplying the flap. A consequence of such damage to the blood supply may result in flap necrosis, delayed healing and potential scarring of the soft tissue.
Flap Repositioning: The flap design should also consider the plan for repositioning the flap after implant placement. The edges of the flap must be approximated again over healthy bone without applying any tension. The flap design should not alter the vestibular depth. In case of inadequate keratinized tissue, the crestal incision should be given more palatally/lingually.
The edges of the flap should lie passively close to each other just before suturing. No significant force should be used to make the edges line up with each other. To ensure close flap adaptation to the underlying bone, the formation of hematoma should be minimized.
Flap Closure: It must be kept in mind that suturing has to be performed with connective tissue opposed to connective tissue to ensure primary closure. If the edges do not line up, the flap must be mobilized by preparing a horizontal periosteal releasing incision. This incision is made at the base of the flap apical to the mucogingival junction. Once the periosteum has been released, the flap can be mobilized and moved coronally and it will then be possible to suture the flap without tension.
Special Considerations for Implants: The flap design must take into consideration the number and location of implants required to replace the missing teeth, and whether the implants are to be inserted in a one-stage or a two-stage procedure. The amount of bone should be assessed clinically and radiographically to decide if the implant can be placed with, or without simultaneous bone augmentation, or if bone augmentation should be performed as a separate surgical procedure. A special esthetic risk assessment should be done before placing implants in the esthetic zone to determine if the flap design needs to be varied to minimize esthetic complications.
Types of Incisions & Flap Designs
Flap designs vary based on the surgical needs and the esthetic requirements of the procedure. Below are some common types:
Horizontal/Crestal Incisions – One-sided flaps
Mid-crestal incisions – Here, horizontal incisions are made in the median position of the ridge. It extends intra-sulcularly around the neighboring teeth.
Indications:
- In posterior areas with sufficient bone volume.
- For buccal and palatal/lingual bone grafting (requires sufficient buccal and palatal soft tissues)
- For stage I and II implant surgery
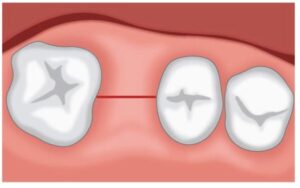
Para median incision – These incisions can be adjusted either buccally or lingually to the mid-crest to maintain keratinized tissue, which is vital for healthy soft tissue outcomes.
Indications:
- Inadequate keratinized tissue
- Implants in esthetic zone
- In bone augmentation procedures alone to facilitate closure of the flaps
- For stage I and II implant surgery
 One Vertical Releasing Incision – Two-sided flaps/Triangular flaps
One Vertical Releasing Incision – Two-sided flaps/Triangular flaps
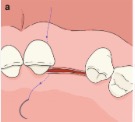
For better access in surgeries requiring bone augmentation, a vertical releasing incision may be added to a horizontal incision to create a two-sided flap. This design ensures adequate visualization and flap mobility. As a rule, a vertical releasing incision must not compromise the blood supply of the flap. Therefore, in general, it is placed anteriorly, and at an angle that ensures a broad base to the flap.
Indications:
- Sufficient visualization of the surgical field in sites with sufficient bone volume
- When only minor bone augmentation is required in conjunction with implant placement
- To be able to mobilize the flap for primary closure using horizontal periosteal releasing incisions.
- To treat minor residual peri-implant defects like fenestration or dehiscence defects occurring after implant placement
Two Vertical Releasing Incisions – Three-sided flaps/Trapezoid flaps
A crestal incision at the palatal aspect is performed together with two vertical releasing incisions. While offering excellent visibility, they may lead to increased bleeding because vessels running from the posterior to the anterior jaw region may be cut when the posterior vertical releasing incision is made.
Indications: For extensive bone augmentation processes, such as block grafts.
Parapapillary/H-shaped Incisions – Papilla Preservation Flaps
The interdental papillae are not included in the mucoperiosteal flap but are left attached to the bone at a width of 1 to 2 mm. This approach may preserve more of the interproximal crestal bone than a wider flap that includes the interdental papillae.
Indications:
- Implant placement in esthetic zone if no simultaneous bone augmentation is expected
- Suitable for the stage II implant surgery where the mobilization of a good amount of tissues may be required
(There are many more such minimally invasive flaps meant specifically for Stage II implant surgery, which are beyond the scope of the present article. However, they will be discussed in great detail in the upcoming issues.)
Periosteal Releasing Incisions
The periosteal releasing incision, or PRI, is a common oral surgical technique that is undertaken to increase the mobility of a surgical flap. Here, the base of the flap is separated from the periosteum by severing the periosteal fibres with the scalpel blade or surgical scissors in a ‘brushing’ movement. Minimum one vertical releasing incision must be given for effectively performing a PRI. When performed correctly, the PRI allows the flap to be coronally advanced so that tension-free primary closure of the surgical site can be achieved.
Indications:
- To increase flap mobility for primary closure
- Guided Bone Regeneration (GBR) procedures in implantology
- In bone augmentation procedures.
Flap Complications
Complications can arise if flaps are not well-designed or handled properly. Common issues include tearing or dehiscence, which can expose underlying bone and implants, leading to pain, bone loss, and prolonged healing. Proper tension-free suturing and careful incision techniques can mitigate these risks.
Esthetic Considerations in the Esthetic zone
In the esthetic zone, preserving soft tissues is paramount. Techniques like parapapillary incisions help in maintaining interdental papillae and reducing scarring potential. Such techniques are crucial for avoiding unsightly black triangles between teeth.
Flap Considerations in Immediate Implant Placement
In extraction sockets, implants must be placed without the elevation of a flap as much as possible. Prerequisites to performing this approach are intact socket walls and a facial bone wall of at least 1 mm in thickness, which must be verified at the time of extraction even if a CBCT scan was taken prior to surgery.
Advanced techniques: Flapless surgery
Flapless surgery, while reducing morbidity and post-operative pain, requires meticulous planning and a high level of skill. This approach is suitable for cases with adequate bone volume and experienced practitioners. It emphasizes the need for three-dimensional imaging and precision.
Conclusion
Successful implant surgery heavily depends on appropriate flap design and meticulous execution. Whether in straightforward or complex cases, effective planning and skillful handling of soft tissues can lead to optimal healing and aesthetic results. For aspiring dental professionals, understanding these principles is indispensable for advancing in the field of implantology.
References
- Merete Aaboe. Principles of flap design in dental implantology. ITI Blog, 2021.
2. Abdulmoein AlFotawi R. Flap Techniques in Dentoalveolar Surgery [Internet]. Oral Diseases. IntechOpen; 2020. Available from: http://dx.doi.org/10.5772/intechopen.91165
- Yashodeep Chauhan, et al. Flap Designing for Dental Implants: A comprehensive review. International Journal of Dental Science and Innovative Research, 2018. 01(03); 23-29
- Jelinek LA, Marietta M, Jones MW. Surgical Access Incisions. [Updated 2024 Oct 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK541018/























Comments