This article is penned down by DentalReach Dental Divas Summit (DRDDS) 3 Speaker Dr Sonal Yerpude.
If you wish to associate with DentalReach or Dental Divas, please get in touch with me – editor@dentalreach.co
Abstract
Full mouth rehabilitation entails a clinician to have an in-depth knowledge of procedures necessary to produce healthy, esthetic, functional, and self-maintaining balanced occlusal system. This article aims to understand the physiology and implications of temporomandibular joint disorders, with its management through appliance therapy and deprogramming prior to full mouth rehabilitation. Keywords: Orofacial pain, Full mouth Rehabilitation (FMR), Temporomandibular joint disorders (TMD), Tooth wear, Attrition, Erosion Parafunction, Deprogramming, Occlusion.
Introduction
Full-mouth rehabilitation (FMR) is a complex dental treatment procedure. The clinician must aim to look beyond the white-pink tissue to achieve not only replacement of the lost tooth structure, but also correction of improper forces acting on the dentition and musculoskeletal system. The key element is restoring lost vertical dimension with a balanced TMJ and occlusal system.
Clinician must understand the overall disruption in stomatognathic system that has attributed for the need of FMR. The assessment must be considered based on multiple factors such as:
- stage of dental wear
- location of wear pattern
- TMJ dysfunction
- co morbidities and
- associated facial features.
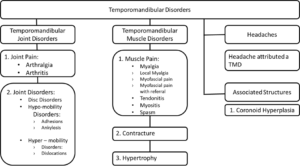
Temporomandibular disorder (TMD) is a collective term used to describe musculoskeletal conditions characterized by pain in the muscles of mastication and temporomandibular joint or both, and/or associated structures. Patients with early signs of wear and little or no co-morbidities or associated features are the best to be manage with regular restorative or orthodontic procedures. In patients requiring FMR, documented TMD prevalence is as high as 10- 12 % and more common in females, although most of the patients with dental wear will show signs of TMD at different level. Clinical representation of TMD is multifactorial and confusing due to convergence phenomenon of the trigeminal system.
A dual-axis system to diagnose and classify patients with TMD, based on the presenting signs and symptoms
Diagnosing a TMD
- CLINICAL ASSESSMENT OF OROFACIAL PAIN
Categorise pain or discomfort into odontogenic and non-odontogenic origin. Collect following data regarding patient history:
- How does the patient describes the pain or issue and its location.
- Onset of the current chief complaint, the duration, and type of pain (throbbing pulsating shock like)
- Snoring or any parafunctional habit, sleep disorder
- Pain exaggerating and alleviating factors.
- Mallampati score or OSA history.
- Medications or any treatments that may have been prescribed – Vitamin Deficiency if any.
RED FLAGS TO BE CONSIDERED
- History of jaw locking, clicking, sudden onset preauricular or postauricular pain, throbbing spasmodic or current shock like pain.
- No odontogenic cause for pain .
- Treatments done for no definitive reasons or undiagnosed pain.
- Chronic periodic or continuous complain of headaches, tinnitus, or sinus pain.
- Facial asymmetry
- Body posture and gait change.
- Fatigue or chronic aches all over the body
- Sudden change in lifestyle
- MUSCLE PALPATION
- Evaluate muscles of mastication and neck muscles for muscle tenderness, hypertrophy and referral pattern.
- Evaluate the Pterygoids with functional manipulation technique.
- CONDYLAR PALPATION
- Palpate the condyles for temperature, asymmetry, pain sounds or unilateral feel of condyles.
- MANDIBULAR RANGE OF MOTION AND DEVIATION
- The range of motion of mandible is measured at active and passive maximum interincisal distance, as well as at the onset of pain.
- Check for deviation and pain or restriction of mandible, during opening and closing of mouth.
- INTRAORAL EVALUATION
- Evaluate dental wear pattern or shifting of teeth.
- Presence of bony changes, linea-alba line, gingival recession or hypertrophy.
- Lateral excursive movements pattern and interferences.
- RADIOGRAPHIC EVALUATION THROUGH PANORAMIC IMAGING
- Check for degeneration of condyles and glenoid fossa, and their inter-relation.
- Dental findings.
- Mandible to maxilla relation.
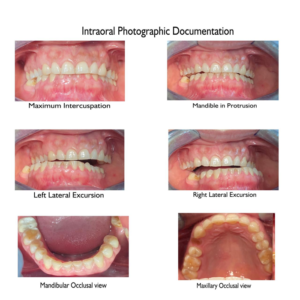
- METICULOUS PHOTO DOCUMENTATION
Pre-op photo documentation.
- Full face regular – three views – straight, left and right.
- Full face smiling – three views – straight, left and right.
- Retracted arch view – straight, left and right.
- Retracted occlusal arch view – upper
Why to Deprogram before FMR?
To understand deprogramming, understand what we are de-programming!
Individual’s developmental stages dictate pre-established pattern (engrams) of neuromuscular and musculoskeletal activity to accomplish daily activities such as
- speech
- swallowing
- chewing
- talking etc.
Any disruptions in this set pattern due to factors such as:
- space occupying lesions
- trauma
- developmental disorders
- environmental exposures
- parafunctional habits
- malocclusion or
- missing teeth
can lead to the positional change in relation of maxilla to mandible which in turn affect the TMJ.
Muscles of mastication such as lateral pterygoids go into hyperactivity and later spasm to perform regular function of mastication or maximum intercuspation leading to condylar disc assembly and the dentition being pushed to an inappropriate position which results in:
- condyle and fossa degeneration
- imbalance in the way condyle seats over the disc
- changes in retro discal tissue and
- wear pattern in dentition.
Most patients have a reflex closure guided by the teeth. Proprioceptive mechanism determines path of mandibular closure and is responsible for awareness of position of mandible in space. To enable the condyles to be placed in an unstrained position, the musculature must first be deprogrammed from its habitual closing pattern.
The lateral pterygoid is the key muscle of mastication which prevents the condylar seating since it is programmed to position the mandible in such a way that avoids pain and posterior interferences in the arc of closure. Deprogramming generally is done by increasing the vertical dimension that prevents posterior teeth contact, allowing the lateral pterygoid to stretch, release and relax. Deprogramming is all about relaxing the muscles and achieving stable TMJ.
When and How to Deprogram before FMR? before FMR?
Most of early stage TMD are self-limiting and do not require any interventions. Usually self-care such as:
- hot and cold fomentation (cryotherapy)
- restricting jaw movements,
- use of soft diets
- jaw exercises
- physical therapy
are enough to take care of symptoms. Chronic pain or discomfort prolonging beyond months or patients showing positive load test should be evaluated for the intensity and treatment options such as:
- pharmacological treatments
- deprogramming and use of removable hard acrylic deprogrammers or stabilising appliances.
The patients who suffer from TMD’s of muscular origin benefit most with the appliance therapy.

Hard acrylic Stabilisation appliance/Deprogrammer
There are various types of occlusal appliance described in the literature; they have different indications and functions. The most used deprogrammer or stabilization or repositioning appliance is a removable appliance that allows the opposing natural teeth to glide over its contact or biting surface. These hard appliances are made using clear acrylic resin covering three fourth tooth structure up to second molars, de-occluding the posteriors and providing space for mandibular anterior teeth to minimally glide. This can control the TMD and help in a better prognosis of your FMR cases.
How do deprogrammers or appliances work?
Deprogrammers or stabilization appliance works in the following ways:
- Increasing the vertical dimension, de-occluding the posteriors thereby relaxing the muscles.
- Allows the condyles to achieve a balance condylar discal relation against the fossa, stabilising the retro discal tissues.
- Reduction in peripheral sensory input to CNS, breaking the parafunctional habit, relieving the symptoms and cessation of hyperactive muscle memory.
- Placebo
It is suggested that patients wear the appliance only at night for 2-3 weeks depending on the severity .
Following deprogramming with appliance therapy, we can ideally aim for most favourable balanced full mouth rehabilitation for a definitive satisfying treatment prognosis.
Conclusion
For most patients seeking FMR showing signs of TMD, before proceeding for any definitive irreversible procedure, deprogramming with muscle modulation and removable appliance helps in achieving a balanced condyle-fossa relationship and stable occlusal scheme.
References
- Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002;72(1):28–35. – PubMed
- Severt TR, Proffit WR. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg. 1997;12(3):171–176. – PubMed
- Fong JH, Wu HT, Huang MC, Chou YW, Chi LY, Fong Y, Kao SY. Analysis of facial skeletal characteristics in patients with chin deviation. J Chin Med Assoc. 2010;73(1):29–34. doi: 10.1016/S1726-4901(10)70018-6. – DOI – PubMed
- Three dimensional evaluation of the skeletal and temporomandibular joint changes following stabilization splint therapy in patients with temporomandibular joint disorders and mandibular deviation: a retrospective study.
- Ahmed MMS, Shi D, Al-Somairi MAA, Alhashimi N, Almashraqi AA, Musa M, Li N, Chen X, Alhammadi MS.BMC Oral Health. 2023 Jan 13;23(1):18. doi: 10.1186/s12903-023-02720-w.PMID: 36639670
- Okeson, J.P. The classification of orofacial pains. Oral Maxillofac. Surg. Clin. North Am. 2008, 20, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Rongo, R.; Ekberg, E.; Nilsson, I.M.; Al-Khotani, A.; Alstergren, P.; Conti, P.C.R.; Durham, J.; Goulet, J.P.; Hirsch, C.; Kalaykova, S.I.; et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for children and adolescents: An international Delphi study-Part 1-Development of Axis, I. J. Oral Rehabil. 2021, 48, 836–845. [Google Scholar] [CrossRef]
- Pathogenesis of TMD. Adopted from Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. The New England journal of medicine 2008;359:2693-705 4.















Comments