The most crucial step towards healing is having the right diagnosis.
Abstract
Odontogenic cysts of the oral cavity can be either developmental or inflammatory in origin. The most common inflammatory odontogenic cyst is the apical periodontal cyst, commonly known as ‘radicular cyst.’ This case report describes an inflammatory radicular cyst of the anterior maxilla which was successfully treated by conventional root canal treatment and endodontic surgery or apicectomy.
Introduction
The radicular cyst, also called as dental root end cyst, is a periapical lesion associated with non-vital teeth in the tooth-bearing regions of the jaws. It has a slight male predilection. It is typically asymptomatic, but if large or secondarily infected, it may cause swelling. The usual radiographic appearance of a radicular cyst is that of a periapical radiolucent lesion.
Approximately 60% of the radicular cysts are found in the maxilla with a propensity for the anterior maxillary teeth.
Etiology – It arises from chronic apical periodontitis, itself the product of root canal infection and pulpal necrosis. The inflammatory cells found in chronic apical periodontitis release cytokines and growth factors which induces epithelial rests of Malassez proliferation. The proliferation of epithelial rests of Malassez leads to formation of a radicular cyst.
This case report describes an inflammatory radicular cyst of the anterior maxilla which was successfully treated by conventional root canal treatment and endodontic surgery or apicectomy.
Case Report
A 26-year-old male patient was referred to the clinic complaining of mild pain in the upper front tooth region for 1 week. Patient gave history of trauma to the front teeth around 10 years ago for which no treatment was performed.
Clinical Findings

21 (Left central incisor):
- Intra oral examination revealed a discolored 21 with slight tenderness to percussion
- Grade 1 mobility was observed
- Responded negative to pulp sensitivity testing
22 (Left Lateral Incisor)
- Normal with no tenderness, responded positively to pulp sensitivity testing
- No evidence of any surface changes/bleeding/sinus opening/pus discharge
Radiological Findings
IOPA Report
- The IOPA revealed well defined periapical lesion involving 21 and 22
- Patient was subjected to CBCT scan for further exploration of the finding, and to check for proximity or any involvement of lesion with nasal floor, since lesion was extensive
CBCT Report

CBCT scan of the patient revealed loss of enamel, dentin and partial pulp structure in mesial aspect of the crown of 21, suggestive of Ellis class III fracture. An ill-defined periapical radiolucent lesion extending upto 22 region distally [9mms], upto the level of middle third of root of 21 inferiorly [13mms] and from labial cortex to palatal cortical plate antero-posteriorly [9mms] was seen.
- Borders were ill defined and irregular with the internal structure being uniformly radiolucent.
- Floor of the nasal fossa and naso-palatine canal were unaffected
- Labial cortical plate was thinned out and breached at the level of middle third of root of 21
No abnormality was reported for 11 or 22.
Radiologic Impression: 21 – Ellis class III fracture with peripaical rarifying lesion
Diagnosis & Treatment Plan
Provisional Diagnosis from these above findings was:
Radicular cyst secondary to trauma in relation to the left maxillary central incisor.
Differential Diagnosis was as follows:
- Nasopalatine cyst
- Globulomaxillary cyst
- Dentigerous cyst
- Odontogenic keratocyst
Treatment Plan
Treatment plan was formulated and after explaining it to the patient, his informed consent was taken.
- Endodontic phase: Endodontic therapy of 21
- Surgical management of the cyst: Cyst enucleation and cavity filling with sticky bone.
- Prosthetic phase for rehabilitation of 21: Cast post with angulation change followed by a full coverage restoration to put the 21 back in alignment
I. Endodontic Phase
Access opening was done followed by thorough cleaning and shaping of 21. After determination of working length and biomechanical preparation, calcium hydroxide intracanal medicament was used for one week. Then, in the next appointment, obturation was completed with cold lateral compaction technique.
The idea was to slightly over-obturate the tooth which will later act as a guide to locate the root apex (due to the severe palatal angulation of the root) during the surgical phase of the treatment.

II. Surgical Phase
After endodontic therapy surgical phase was carried out.
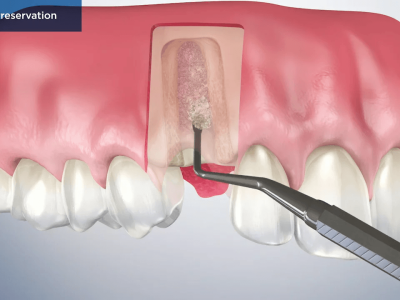
Incision & flap reflection: Bilateral infraorbital and nasopalatine nerve block was given with lignocaine with 1:80,000 adrenaline and a full thickness mucoperiosteal flap was raised from mesial of 12 to mesial of 23.
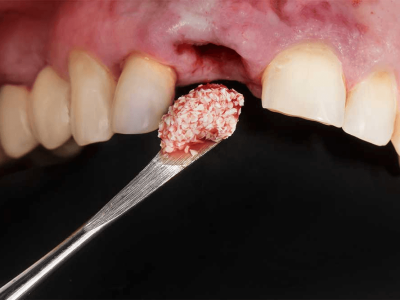
Curettage & Burnishing: Peri-radicular area of 21 and 22 was exposed and overfilling of gutta percha helped in getting access to the root end which was removed and burnished against the root apex. A dental curette was used to peel off the connective tissues wall of the specimen from surrounding bone and then the bony cavity was inspected after irrigation with sterile saline. Complete curettage, along with granulation tissue removal and enucleation of cystic lesion was done and it was sent for histopathological evaluation.
Graft placement & flap repositioning: The osseous cavity was thoroughly irrigated and sticky bone was placed in the cavity to aid in healing. (Sticky bone is a stable fibrin bone graft, obtained by mixing PRF fibrin and liquid PRF with the bone graft granules which results in the formation of sticky, coated bone particles easy to work with in the surgical area.) The flap was repositioned and then sutured.
Patient was kept under observation for the healing of the cystic space.


Histopathology Findings
Histopathological examination revealed a cystic cavity lined by non-keratinized stratified squamous epithelium arranged in an arcading pattern, interspersed with intense inflammatory cell infiltration consisting chiefly of lymphocytes and plasma cells. The histopathological findings confirmed the provisional diagnosis of radicular cyst.
Final diagnosis – Radicular cyst secondary to trauma in relation to the left maxillary central incisor.
III. Prosthetic Phase
Tooth preparation was done in accordance with new core position in alignment. Post-space preparation was done with Peeso Reamer #2 and the canal was circumferentially filed for even and smooth inner surface receptive of taking a wax pattern.
An impression of the canal was taken with the help of #40 K file and inlay wax which was then given for casting. The file was angulated to the future position of the core to straighten the tooth in alignment with the rest of the arch.

The custom cast post was then cemented and an impression was taken for the final crown which was then cemented in line with the rest of the teeth in the arch.
Although the angulation was severe, we were able to achieve decent esthetic results.

Follow Up
- Post-operative instructions were given to the patient and patient was kept on antibiotics and analgesics
- After six months, both clinical and radiographic evaluation was very satisfying with complete resolution of all clinical symptoms

Currently, the patient is asymptomatic and he is under follow-up for the past 2 years


Discussion
Radicular cysts are thought to be formed from epithelial cell rests of Malassez (ERM), which are remnants of Hertwig’s epithelial root sheath, present within the periodontal ligament. Proliferation of these epithelial cell rests is frequently associated with stimuli from periapical periodontal inflammation secondary to pulpitis. The treatment modalities of radicular cyst are either root canal therapy when lesion is localized or surgical treatment like cystic enucleation, marsupialization or decompression when lesion is large. In our case, we preferred enucleation and endodontic treatment and saw good results after the 2 year follow up.
Formation & growth: During periapical inflammation, host cells in the periapical tissues release many inflammatory mediators, proinflammatory cytokines, and growth factors which induce proliferation of the ERM in all directions to form a three-dimensional ball mass. As the epithelial mass grows, the central cells move further away from their source of nutrition and undergo necrosis and liquefaction degeneration, forming central cystic cavity lined by epithelial wall. Following its formation, radicular cysts grow by periapical bone resorption mediated by prostagladins and cytokines. It is interesting to note that most inflammatory mediators which induce proliferation of epithelial cell rests also mediate bone resorption in inflammatory periapical lesion.
Differential diagnosis between periapical granulomas and radicular cysts is an important subject to decide on the treatment. Radiometric analysis of radiographs of periapical granuloma and radicular cysts are used to differentiate the two lesions; according to the current literature, size of radiolucencies of periapical granulomas could differentiate these lesions. It has been reported that radicular cysts could be distinguished from periapical granulomas based on the larger size of radicular cysts (more than 5.9 mm). Periapical abscess was ruled out due to the absence of drainage from the canal on initiating root canal treatment. Given the dimensions of the lesion as reported by CBCT analysis, our provisional diagnosis was a radicular cyst, which was confirmed by histopathological analysis.
Provisional & final diagnosis: Radiological analysis is important for provisional diagnosis, in this case, we decided to go radiology beyond the conventional IOPA. Cone beam computed tomography was preferred because the surgeon can assess the exact extension of the lesion, plan the surgical protocol and monitor the results. Since lesion was extensive, CBCT also allowed a check for proximity or any involvement of lesion with nasal floor. Histopathology is essential for final diagnosis. Microscopy gives the exact picture of the lesion, showing its true characteristics. The histopathological findings confirmed the provisional diagnosis of radicular cyst in this case.
Need of Endo-surgery: Proper endodontic therapy of the involved teeth removes irritants in the canals by chemo-mechanical instrumentation. As the root canal is completely sealed, all cell components participating in inflammatory reaction gradually resolve. But if the irritants and inflammatory mediators are in abundance in the periradicular area, treatment of this area directly by curettage and graft placement becomes necessary. This is where micro-surgery or apicectomy comes into play. When the flap is raised, the lesion can be viewed directly and treated completely.
In this case, we used sticky bone to fill the osseous defect. The use of an osseograft combined with concentrated growth factors (CGF) has numerous advantages owing to the formation of sticky bone. The product thus formed can be molded, prevent both macro and micro movements, also the network is proven to contain platelets and growth factors thereby contributing to accelerated soft-tissue healing and bone regeneration. Furthermore, the fibrin interconnection prevents the ingrowth of soft tissue into the bone graft as well.
Studies recommend the placement of root-end filling especially when an unsuccessful root canal therapy was corrected by an apicectomy rather than by re-treatment. In this case, since it was the non-vitality of the tooth due to the long-standing trauma that caused the cyst, it was decided to simply remove the overextended gutta percha, clean and burnish the root apex.
Conclusion
Radicular cyst is one of the most common lesions seen in dental practice . It is most identified incidentally, following radiographic examination. Since there is a high chance of neoplastic transformation, it is advised to carry out proper treatment and follow up patients diagnosed with radicular cyst.
References
1. Nair PN. New perspectives on radicular cysts: do they heal? International Endodontic Journal. 1998; 31:155-60.
2. White SC, Pharoah MJ. Oral Radiology; principles and interpretation. 6th edition; 343-46.
3. Kramer IRH. Changing views on oral disease. Proceedings of the Royal Society of Medicine. 1974;
4. Kadam NS, de Ataide IDN, Raghava P, Fernandes M, Hede R. Management of Large Radicular Cyst by Conservative Surgical Approach: A Case Report. Journal of Clinical and Diagnostic Research. 2014; 8(2):239-41.
5. Chkoura, A., Wady, E. W., & Taleb, B. (2013). Massive Radicular Cyst Involving the Maxillary Sinus: A Case Report.International Journal of Oral and Maxillofacial Pathology, 4(1), 68-71.
6. Chaudhary, C., Ravishankar, M., Yadav, A., & Yadav, G. (2012). Healing Of Bone Defects By Autogenous Platelet Rich Plasma In Pediatric Patients. Journal of Recent Advances in Applied Sciences, 27.
7. Freedland, J. B. (1970). Conservative reduction of large periapical lesions. Oral Surgery, Oral Medicine, Oral Pathology, 29(3), 455-464.
8. Doan N, Nguyen-Pham L, Liang C, Duong QT. A review on the application of concentrated growth factors and MPhi laser to regenerate oral defects in the oral and maxillofacial region and a two cases report. Int J Oral Maxillofac Surg. 2017;46:203–4
9. Shrout MK, Hall JM, Hildebolt CE. Differentiation of periapical gran- ulomas and radicular cysts by digital radiometric analysis. Oral Surg Oral Med Oral Pathol. 1993;76(3):356–61.
10. Róz ̇yło-KalinowskaI.Digitalradiographydensitymeasurementsin differentiation between periapical granulomas and radicular cysts. Med Sci Monitor. 2007;13(1):129–36.
















Comments