Abstract
Chronic inflammation due to periapical abscess can drain into the mouth or outside on the skin through a sinus tract. It may be difficult for the general physician to differentiate the opening of the fistula from primary skin conditions who wrongly refers patients to dermatologists. This is a case report of a chronic periapical abcess with draining fistula, where the delayed diagnosis caused a great deal of misery to patient, who was heavily pregnant during the Covid lockdown.
Introduction
Periapical abscesses due to cavities or trauma commonly cause intraoral fistulas, and less commonly cause extraoral fistulas, which drain directly onto the skin. Extraoral fistulas are rare and many times misdiagnosed as skin lesions. This misdiagnosis is further treated with an unnecessary antibiotic therapy, allowing the infection to become chronic and the abscess to become a hard swelling.
Whenever a patient has a facial fistula, it is mandatory to have a complete oral exploration looking for an odontogenic abscess besides the fibrous tissue/fistula. It is necessary to corroborate the periapical infection with a panoramic x ray, or it may be done by drawing the sinus tract with radiopaque material such as gutta percha, and then shooting the x-ray. Therapy consists of treating the underlying infection, either by endodontic treatment of teeth which can be saved, or if the the tooth is totally broken down, it is best to remove it.
This article describes the case of a patient who was treated by a physician and then a dermatologist, but with no improvement in lesion since it was misdiagnosed.
A personal note
This case will stay close to my heart. During the coronavirus pandemic, the whole nation was shut down and so was our clinic. My clinic is an extension of my house campus. It had been two months of lock down period when a young lady appeared in my clinic from a village. She was pregnant and had a huge swelling on her face. So when she rang the bell, looking at her condition, we could not send her back.
My husband and myself, both of us being dentists, had a brief discussion on what to do. In fact I would say an argument! I was honestly a bit relucatant to take up the case – the staff was on leave, it was peak covid time and she had travelled from a nearby village. But it was time to fulfill our ethical duty and do the needful for her, because she was literally on verge of crying. She had been refused by all hospitals nearby, none of the private practitioners attended her and all refused to examine her. After some dilemma we decided to let her in and treat it as an emergency, atleast relieve her from her swelling.
Case Report
A 25 year old female patient reported to the clinic with a chief complaint of a huge swelling on the left side of her face.
History: She gave a history of a cheek lesion which was diagnosed as a skin problem by the local physician, who referred her to a dermatologist in a village near by. She was prescribed oral medications (antibiotics) and local ointment by the dermatologist, but she got no relief. She was 7 months pregnant, with no history of pre-eclampsia or gestational diabetes mellitus.

Examination: On oral examination, in 36 region, she had root stumps and there was huge abscess in relation with that tooth, leading to an extraoral fistula. It was primarily diagnosed as a dental problem and not a skin problem.

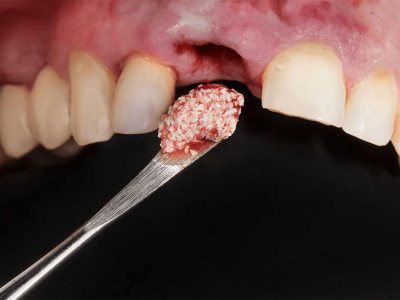
Emergency treatment: As the patient was already under an antibiotic cover, a usual incision and drainage was performed of the abscess extra orally. There was a huge amount of pus exudate and she instantly felt relief. Since the root stumps had poor prognosis, it was decided to extract them to eliminate the focus of infection and provide healing.
She was told to to consult her gynecologist and take her consent for extraction under local anesthesia .
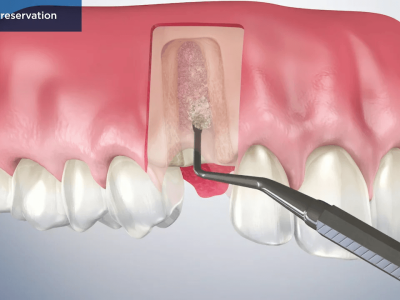
Surgical treatment: After 3 days, the patient re-visited the clinic, this time with an appointment, and with the gynecologist’s approval and consent on paper. The root stumps were extracted under local anesthesia in an atraumatic manner. Curettage was done of the periapical area, followed by copious irrigation with saline and betadine. The patient was instructed to keep strict oral hygiene. No packs or special treatment was done for the fistula as it was small and was expected to heal on its own. Since the patient was already under an antibiotic cover, she was only prescribed analgesics which were safe for use in pregnancy.
Follow-up: A telephonic follow-up after a week revealed that she had no pain, discharge or swelling and the fistula had closed. One month after her delivery, she visited the clinic. Her face had no scar and the fistula had healed completely. Prosthetic rehabilitation was explained to her, which she decided to opt for after a few months.
Discussion
Cutaneous dental fistulas are not a common dermatological subject, which is why it is misdiagnosed by dermatologist and surgeons, thus submitting the patient to unnecessary antibiotic treatments, biopsies, resections, and even radiotherapy, with a not so favorable outcome and a recurrence of the fistula.
Initially, microorganisms such as Fusobacterium nucleatum sp. Vicentii, Porphyromonas gingivalis, Veillonella parvula, Enterococcus faecalis, Campylobacter gracellis and Neisseria mucosa invade the tooth through the enamel and dentin, infecting the pulp causing necrosis, periodontitis and formation of the periapical abscess, rich in anaerobic bacteria. Usually this process is acute and renders the patient to seek medical attention. At this point, the purulent material finds a way out through an abnormal canal that connects the alveolar abscess with an orifice in the interior of the mouth (intraoral sinus tract), or into the skin (extraoral sinus tract).
Based on a recent report, extraoral fistulas are more common in women and adults and intraoral fistulas are usually found in children. The draining pathway depends on the length of the root and the exposition of the apex, in relation to the muscle union to the bone.
The purulent material tries to find a way out through a place that presents less resistance, in order to relieve the pain and the edema.
The purulent material does this by passing through the periodontal ligament, bone and soft tissue right into the epidermis, creating abscess or cellulites of the skin, which leads to a hole in the skin. Besides caries being the most common cause of periapical infection, there can be other causes such as trauma and root retentions. Clinically, there can be a soft nodule on the skin, symmetric, erythematous, or covered with scab tissue, the skin can be retracted because of a fibrous tissue that joins the jugal mucosa with the gingival tissue, which if it is palpated may produce the exit of purulent material.
The most common fistulas are associated with mandibular teeth. Topically, they are localized in the angles of the mandible, chin and cheeks, and most of the times it can be predicted where the fistula will drain, depending on what tooth is affected: the mandibular premolars and molars will drain into the submandibular regions and some into the cheek of the affected side.
The diagnosis of a fistula requires a well taken medical history and adequate physical and oral examination. Past inflammatory process and dental work should be asked about. The panoramic or periapical x-ray may show some radiolucent areas, traces with gutta percha on the sinus tract (radiopaque material is put into the fistula and then the x-ray is taken to determine the source of infection). If there is purulent material it is best to take samples for cultures, in 60% of the cases it may be caused by anaerobic bacteria.
Treatment consists of the elimination of the infectious agent through endodontic work if the tooth can be saved. If it cannot, it is best to remove it. Patient should be under a cover of systemic antibiotics. Once the infection is treated, the sinus tract heals in 5-14 days and closes by secondary intention. The esthetic results, however, are determined by the size. Small sized fistulas heal on their own. In medium and big sized fistulas, the results are not so favorable; patients present with scaring and depressions of the skin. Hence, the medium sized ones should be sutured, while big sized ones should be surgically removed.
Conclusion
An initial dental consultation would have avoided this patient an unnecessary dermatology visit, and instead she could be directly referred to dentist. General physicians and dermatologists must be made aware of this overlapping condition. Emergency treatment should be considered in acute conditions and final treatment must be postponed till acute condition subsides. It is best to have all consents and physicians approvals in place, especially in compromised patients and states like pregnancy.
A stitch in time saves nine, so right diagnosis at right time is crucial.














Comments