Editorial for DR OMFS Special (Volume 5, Issue 9)
Restore more than smiles in broken homes…the uncomfortable truth of domestic violence must be uncovered by the ethical dentist.
We focus on head and neck injuries of athletes or military veterans, but victims of domestic violence comprise an under-represented group.

An article from Journal of Aggression, Maltreatment and Trauma, reports that 75% of head and neck trauma associated with domestic violence, occurs with oral injury. Researchers have concluded that dentists are in the unique position to probably be the first and only health professional to evaluate a domestic violence victim.
Yet, dentists receive no education about identifying and discussing domestic violence with potential victims.
It is estimated that more than 4.8 million women are assaulted annually worldwide.1
Statistics show as rage, frustration and stress grows, men are also being subjected to violence.
An astonishing 2.9 million men are victims of intimate partner violence. 1
Violence between children, elderly and same-sex partners is also being seen.
The problem is more common than we assume, and it is possible that we are interacting with such patients on a daily basis – but it does not cross our mind.
Did you know that head and neck trauma is most common in domestic violence?
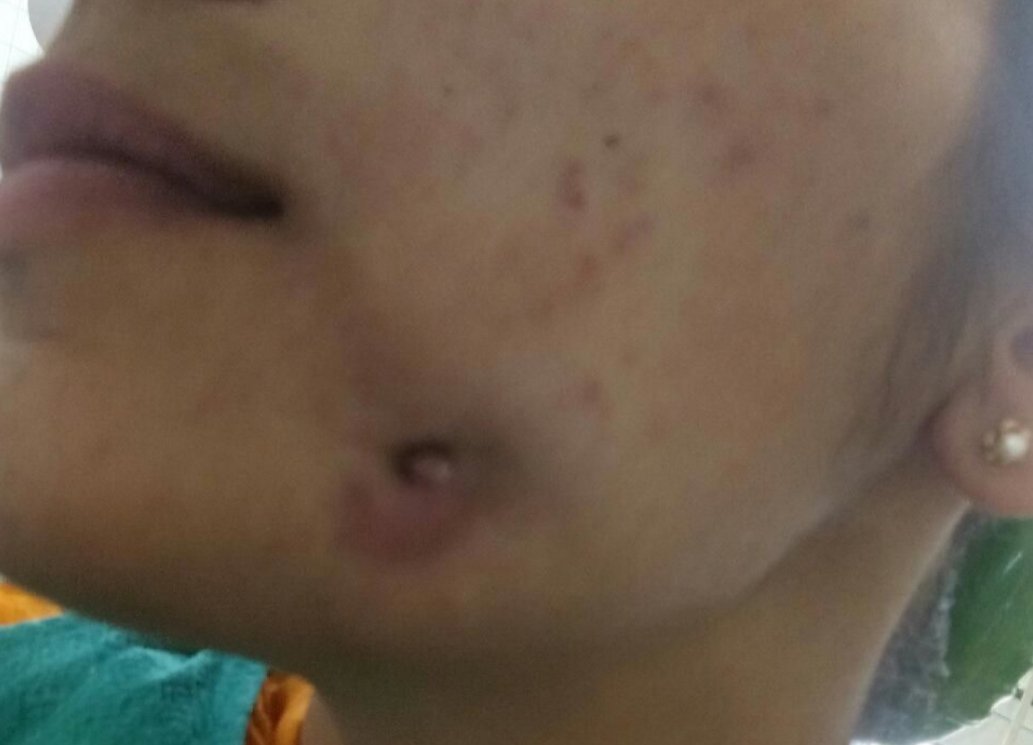
A number of studies have shown that the head and neck are the most frequently injured areas in abused patients, resulting in fractures, traumatic brain injuries, burns and traumatic dental injuries.
The aggressor's preference for the face of the victim can be associated with the symbolic nature of humiliation that this kind of violence represents. When women are attacked, face aggression is associated with the aggressor's intention of damaging a socially appraised attribute: a woman's beauty. The head is the most exposed and accessible body area that represents the individual. This region of injury can direct or indirectly devastate the victim's life by affecting their appearance and communication, and cause functional, esthetic, psychological and social problems.
Oral biomarkers of domestic violence
The oral biomarkers that could help dentists potentially identify domestic violence victims are majorly traumatic injuries of teeth.
A dental study in Brazil 2 collected data of domestic physical aggression from police records. The aggression in all cases occurred in the form of punches and slaps. There was a predominance of individuals with head and neck injuries and the frequency of traumatic tooth injuries was 2%. The most frequently injured teeth were maxillary incisors, followed by mandibular incisors and maxillary canines. Of the dental trauma cases, 59% were tooth fractures, 27% were luxations and 13% were avulsions. In conclusion, domestic violence was an uncomfortable, yet important etiologic factor of traumatic dental injury.
Child Abuse
According to the American Academy of Pediatrics, over 2.5 million cases of child abuse and neglect are reported each year.
A study in Arabia 3 assessing the occurrence of trauma in students, pointed that domestic violence was the second most common cause of injury. They highlighted that as information was obtained from the children's parents, it may even be the top common cause, since parents may not confess towards the true degree of aggression against their own children. Children's abuse was seen as contusions, burns or laceration of the tongue, lips, oral mucosa, palate (hard and soft palate), alveolar gingiva and frenum, injuries to the facial bones, and mandibular fractures.
Dental neglect
Dental neglect may be an indicator of domestic violence. The aggressor typically doesnot care enough for the victims to get their treatments done or restricts them from seeking help or health care. The victims may not have the confidence to approach a health care facility on their own and may be too mentally and physically exhausted to undertake a strict and consistent oral hygiene regime at home.
Routine conditions showing dental neglect, which may at times be related to domestic violence are:
- untreated decay
- facial pain
- lesions in the mouth
- long standing cases of complete edentulousness
- new and old facial bruises or
- facial lacerations.
How to diagnose – Clinical signs & symptoms of domestic violence
When injuries are seen in cases with no proper history and severe signs and symptoms, the likelihood of abuse should be strongly suspected 4:
- Missing or avulsed teeth
- Unexplained oral trauma
- Bruises, both old and new
- Lacerations in the mouth or around the face
- Neck trauma, including marks or bruises
- Evidence of trauma or scarring in the perioral area
- Lesions in the mouth
- Unexplained orofacial pain
- Untreated or rampant decay
Additional Clinical Signs of Domestic Violence 4:
- Intraoral bruises from slaps or hits when soft tissues are pressed against hard structures such as teeth and bones.
- Patterned bruises on the neck from attempted strangulation such as thumb bruises, ligature marks, and scratch marks.
- Petechiae bruising in the face, mouth, or neck caused by attempted strangulation.
- Soft or hard palate bruises or abrasions from implements of penetration (may indicate forced oral sexual acts)
- Torn frenum (may be the result of assault or forced trauma to the mouth)
- Fractured teeth, nose, mandible, or maxilla. (Signs of healing fractures may be detected in panoramic radiographs.)
- Abscessed teeth (caused by blows to an area of the face or from traumatic tooth fractures)
- Bite marks
- Hair loss (from pulling), black eyes, ear bruises, or lacerations to the head
- Injuries to arms, legs, and hands noted during the dental visit.
Behavioral indicators
The history is inconsistent and injuries are usually unexplained or explanations are not convincing. The accompanying person provides different explanations about how the injury has occurred and there would be a history or evidence of similar injuries. There would be a delay between the time of injury and the time at which the person is brought in for care.
Psychologic indicators
The psychologic indicators are avoidance, fear, anxiety, low self-esteem, and depression. The psychologic indicators are usually clearly visible and the victim is highly withdrawn. The body language between the accompanying person and patient will be tensed.
Diagnostic checklist for the dentist
It is important to distinguish abuse from accidents, because the clinical signs and symptoms may be the same. Here is a checklist that would be helpful in diagnosis:
- Is the injury inconsistent with the given history or explanation of the cause?
- Is the explanation of the injury inconsistent with the physical findings?
- Is there evidence of previous or repeated trauma?
- Are there multiple skin lesions or bruises that are strongly suggestive of abuse?
- Does the parent or child show inappropriate behavior?
- Is there evidence of neglect or poor supervision?
- Is there hesitation in history taking as if wanting to say more?
If the answer is “Yes” to more than 4 questions, you know you are dealing with a potential domestic violence victim.
What can an ethical dentist do?
Dentists who suspect or recognize some form of abuse have a responsibility of reporting it to the concerned authorities.
Courts have declared “any physician who fails to identify and report a child with historical, physical, and radiological findings that indicate abuse, is guilty of professional negligence.” 5
Whenever suspicions of abuse arise, a routine protocol should be followed, which includes questions about patient history and how the accident occurred, and all relevant information should be documented with radiographs, photographs, and impressions when necessary. Document these before reporting:
- The size, shape, location, color, degree of healing of the injury
- Detailed notes of behavioral indicators
- Pictures drawn of the injured area and labeled accordingly and radiographs of affected teeth
- Photographs of suspicious pathology
What if I’m unsure and don’t wish to report?
- If you still feel hesitant to report, at least refer the patient for medical evaluation and treatment, preferably to a government hospital who deal with such cases on a daily basis and are well trained in protocols.
- Be specifically empathetic to such patients; a listening ear and a good conversation may infuse some strength and confidence into the victim.
- Prioritise them in appointments.
- Finish off their treatments in minimum sittings, because you may not see them again.
- Reinforce the importance of self-care and oral health regimen, provide them with free samples, if any.
Symptoms of domestic violence may initially appear mild, but underlying injuries may kill the victim later. Identification, intervention and quick action to refer the patient for medical evaluation and treatment (if not reporting to authorities), can save a life.
Helpline numbers
India:
- Toll-free to support woman in distress – 181
- National Commission for Women Helpline – 7827170170. http://www.ncw.nic.in
- National Human Rights Commission -(011) 23385368/9810298900. https://nhrc.nic.in
- Helpline for men in distress (Daaman) – 8882-498-498 https://www.daaman.org
- Indian state-wise helpline list: https://indianhelpline.com/WOMEN-HELPLINE/
USA:
- National Domestic Violence Hotline: 800-799-7233 (SAFE) 800-787-3224 (TTY) www.ndvh.org
- Rape, Abuse, and Incest National Network (RIANN): 800-656-4673 (HOPE)
www.rainn.org - National Sexual Violence Resource Center (NSVRC): 877-739-3895
www.nsvrc.org - National Teen Dating Abuse Helpline: 866-331-9474, 866-331-8453 (TTY) www.loveisrespect.org
(Since most of our readers are from India & USA, I have provided helpline numbers of these countries. If you belong to any other country and wish to report domestic violence, a quick Google search for any national helpline will help.)
Conclusion
The dental field can become a leader in branding the procedures, protocols, and clinical practices in the recognition and intervention against head and neck injuries in the domestic violence population. We can be the first line of defence in identifying evidence of assault, and then reporting potential cases of domestic violence.
References
1. Zeitler DL. The abused female oral and maxillofacial surgery patient: treatment approaches for identification and management. Oral Maxillofac Surg Clin North Am 2007;19:259-265
2. Garbin CA, Guimarães e Queiroz AP, Rovida TA, Garbin AJ. Occurrence of traumatic dental injury in cases of domestic violence. Braz Dent J. 2012;23(1):72-6.
2. 3. Sgan-Cohen HD, Yassin H, Livny A. Traumatic dental injury among 5th and 6th grade Arab schoolchildren in Eastern Jerusalem. Dent Traumatol 2008;24:458-461.
4. Shanel-Hogan. CDA Foundation. 2004. Retrieved August 2011
5. Mouden LD, Bross DC. Legal issues affecting dentistry’s role in preventing child abuse and neglect. J Am Dent Assoc. 1995;126:1173–80
























Comments