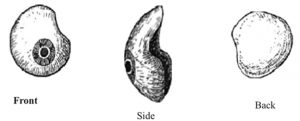
An artificial eye which is also known as ‘Ocular Prosthesis‘ or a ‘Glass Eye‘. It is a kind of craniofacial prosthesis which replaces a missing natural eye after an enucleation or evisceration procedures. This convex shell shaped prosthesis snuggly fits over an orbital implant and is placed under the eyelids. Though it is referred to as a glass eye, the ocular prosthesis is made of medical grade plastic acrylic. Nowadays, some of the ocular prosthesis are made of cryolite glass.
There is a variant of the ocular prosthesis which is like thin hard shell and popularly known as ‘Scleral Shell’ which can be worn over a damaged or eviscerated eye. Makers of Ocular Prosthetics are known as Ocularists. An ocular prosthesis does not provide vision; but visual prosthesis does provide vision. Someone with an ocular prosthesis is totally blind on the affected side and has monocular or one-sided vision.
Surgical Procedure
- Anesthesia
- Conjunctival Peritomy/Separation
- Separate the anterior Tenon’s fascia from Sclera
- Pass sutures through the rectus muscles
- Rectus muscles are then disinserted from the globe/eyeball
- Rotate and elevate the globe
- Tenon’s capsule is then opened to visualize optic nerve
- Necessary blood vessels are cauterized
- Divide the nerve
- Remove the eye
- Hemostasis needs to be achieved with either cautery or digital pressure.
- Insert orbital implant (parallel to the frontal plane of the face or slightly inward)
- If required cover the implant surface with wrapping material before
- Then the muscle (if possible) is attached either directly (PP) or indirectly (HA) to implant.
- Create fenestrations in wrapping material if necessary
- For HA implants drill 1 mm holes at muscle insertion site
- Draw Tenon’s fascia over implant
- Close Tenon’s fascia in one or two layers
- Suture conjunctiva
- Temporary ocular conformer is inserted until prosthesis is received (4–8 weeks later)
- After implant vascularisation is completed an optional secondary procedure can be done to place a couple peg or post. This post is an extension and can be inserted into a corresponding groove in the back of the ocular prosthesis to improve motility for a natural appearance.
Following procedures also done under anesthesia
- Create conjunctival incision at the peg insertion site
- Hole is created into implant to insert peg or post
- Prosthesis is modified to receive peg/post.
Types of Implants

Nonintegrated Implants
Although there is evidence which shows that ocular implants were invented thousands of years back, modern non-integrated spherical implants came into existence around 1976. Nonintegrated implants do not contain any unique apparatus for attachment to the extraocular muscles and resist ingrowth of organic tissue into their inorganic substance. These implants do not have direct attachment to the Ocular Prosthesis.
Integrated Implants (Porous)
Porous nature of integrated implants allows fibrovascular ingrowth within the implant and insertion of pegs or posts. Direct mechanical coupling is thought to improve artificial eye motility, and these integrated implants are directly connected to the artificial eye. Currently, porous implants comprise of natural and synthetic hydroxyapatite, aluminium oxide, and polyethylene.
Implant Movement
Implant and prosthesis movement are important aspects in the surface appearance after enucleation. They are essential for making a realistic eye similar to the normal fellow eye. There are several theories of improved eye movement, which are using integrating prosthetic material like pegging the implant, covering the implant or suturing the eye muscles to the prosthetic implant.
The proficiency of steering movement from the implant to the prosthesis controls the grade of prosthetic motility. Movement is transferred from old-fashioned nonporous spherical implants through the surface tension at the conjunctival–prosthetic interface and movement of the fornices.
Quasi-integrated implants having irregularly shaped surfaces can create an indirect coupling mechanism between implant and prosthesis, reporting greater movement to the prosthesis. Directly integrating the implant through an external coupling mechanism is expected to improve motility.
What are the two forces which promote movement of a nonintegrated prosthetic eye?
1. The rubbing force between the posterior surface of the glass eye and conjunctiva which covers the implant may cause artificial eye to move. Since this force is likely to be almost equal in every directions, it would cause comparable horizontal and vertical artificial eye movement.
2. An artificial eye fits snugly in the conjunctival space. Therefore, any movement of the conjunctival fornices will be causing the same movement of the glass eye, while lack of movement of the fornices will stop its movement. Imbrication of the rectus muscles over a non-integrated implant provides movement to the implant and prosthesis.
The prosthesis represents a ball and socket joint and moves whenever the implant moves. But, because the ball and socket are separated by layers of Tenon’s capsule, layers of muscles, and the conjunctiva, the mechanical efficacy of transmission of movement from the implant to the prosthesis is below optimal.
Moreover, it is concerning that imbrication of the recti muscles over non-integrated implants can result in implant migration. The recent technique of myoconjunctival enucleation is surely an alternative to muscle imbrication.
Tears Production in Prosthetic eye

There are various factors responsible for prosthetic eye to cause more tears than the natural eye. The primary reason to experience eye discharge is due to anophthalmic, absent eye socket. Similar to the inside lining of the nose or mouth, the prosthetic eye socket is a contiguous mucus membrane; producing considerably larger amounts of fluid than the natural eye socket.
Tearing is body’s natural mechanism for lubricating the surfaces and thereby reducing friction and clearing away debris. In order to counteract with the hydrophobic and water repelling nature of the prosthetic eye material the body itself produces more oily tears to increase lubrication and promote normal eyelid function. With due amount of time an oily layer can accumulate on the surface of the prosthesis and can cause irritation and diminished cosmesis.
To eliminate the formation of eye discharge on the surface of the prosthetic eye, it is really important for the patient to follow his/her ocularist guidelines.
Conclusion
Loss of an eye inflicts both physical and psychological trauma to the patient. The disfigurement resulting from loss of an eye can cause significant psychological as well as social consequences. A thorough knowledge of the regional anatomy and recent developments in the field is judicious. One needs to be a little artistic and very innovative to treat such patients, utilizing the available materials and techniques. Above all, empathy towards the patient’s condition must be present.
References
- Doshi P, Aruna B: Prosthetic management of patient with ocular defect. Journal of Indian Prosthodontic Society. 2005, 5:37-8.
- Ocular Prosthesis. (2011). Accessed: Feb 13 2012: http://en.wikipedia.org/wild/Ocular_prosthesis.
- Sajjad A, Ocular Prosthesis – A Simulation of Human Anatomy: A Literature Review. Cureus 4(12): e74. doi:10.7759/cureus.74



















Comments