Low Level Laser Therapy (LLLT) in Dentistry
This article is penned down by DentalReach Dental Divas Summit (DRDDS) 3 Speaker Dr Mohini Daultani.
If you wish to associate with DentalReach or Dental Divas, please get in touch with me – editor@dentalreach.co
INTRODUCTION
Low-level lasers (LLL) emit short-wavelength red or infrared light with a low water absorption power that can reach a depth of 3 mm to 15 mm in both soft and hard tissues.
 Fig 1: Low Level Laser Therapy
Fig 1: Low Level Laser Therapy
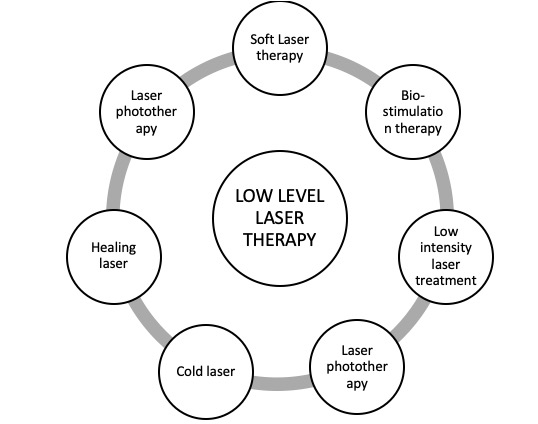
SYNONYMS
 HISTORY
HISTORY
The use of low intensity laser radiation for therapy was pioneered by Endre Master in Hungary in the late 1960s and independently by Fredrich Plog in Canada.
 Fig 2: Fredrich Plog
Fig 2: Fredrich Plog
The first biostimulation laser to be sold commercially was a 1-mW helium-neon (HeNe) laser.
 Fig 3: Helium Neon Laser
Fig 3: Helium Neon Laser
PROPERTIES
- Laser type: Cold Laser: No thermal effects
- Class 1M laser: has the power of class IV laser
- Battery powered hand held device: 18 hours on one charge
- Frequency hertz:5Hz to 50Hz
- Semiconductor laser: Amplifying medium- Gallium arsenide
- Wavelength: 600 to 1000nm red or near infra red beam Non-ionizing
MECHANISM OF ACTION
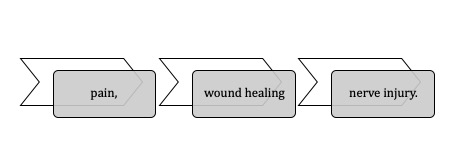 LLLT has been demonstrated to aid in the management of:
LLLT has been demonstrated to aid in the management of:
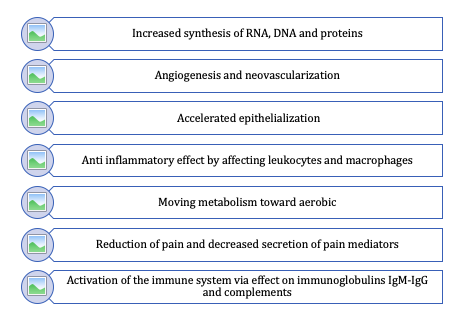
The biostimulatory activity of laser irradiation results in physiological, metabolic, and functional changes in living microorganisms.
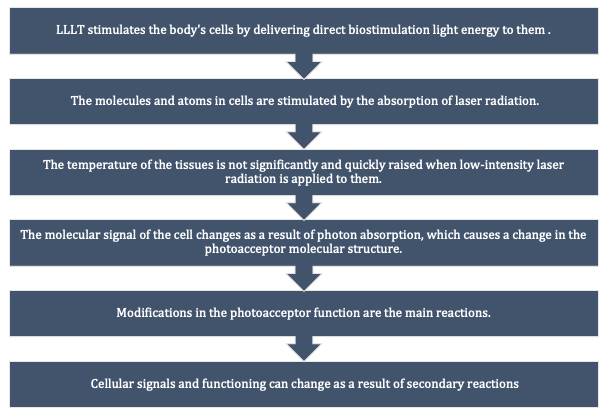
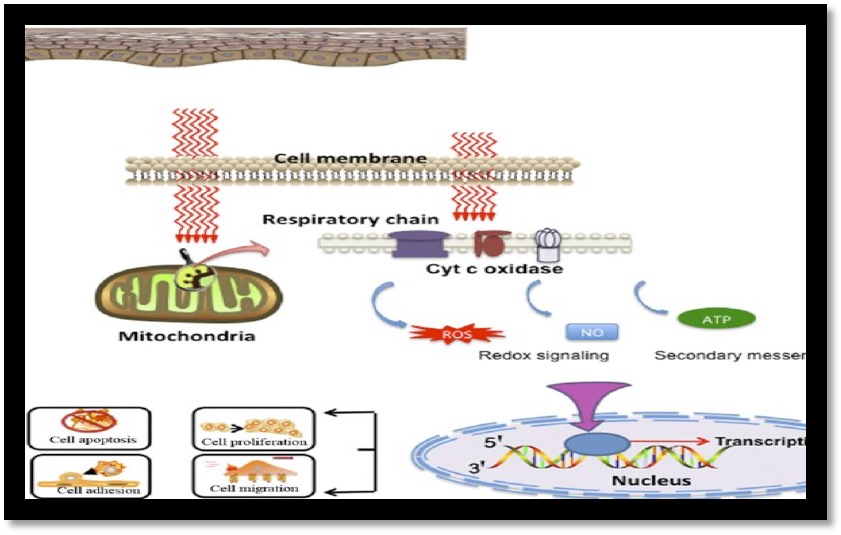 Fig 4: Incoming red and near infrared photons are absorbed in cell mitochondria, producing reactive oxygen species (ROS) and releasing nitric oxide (NO), which leads to gene transcription via activation of transcription factors (NF-kB and AP-1)
Fig 4: Incoming red and near infrared photons are absorbed in cell mitochondria, producing reactive oxygen species (ROS) and releasing nitric oxide (NO), which leads to gene transcription via activation of transcription factors (NF-kB and AP-1)
APPLICATIONS OF LLLT IN DENTISTRY
1) DENTIN HYPERSENSITIVITY
Mechanism: LLLT affects at the cell level to the prevention of the signal transmission of pain from peripheral to central parts as well as blocking of the depolarization of sensory C fiber.
 Fig 5: Laser therapy can be used for decreasing dentin hypersensitivity
Fig 5: Laser therapy can be used for decreasing dentin hypersensitivity
2) POSTOPERATIVE PAIN MANAGEMENT
LLLT seems to be an effective and nonpharmacological approach for the reduction of post-endodontic treatment pain.
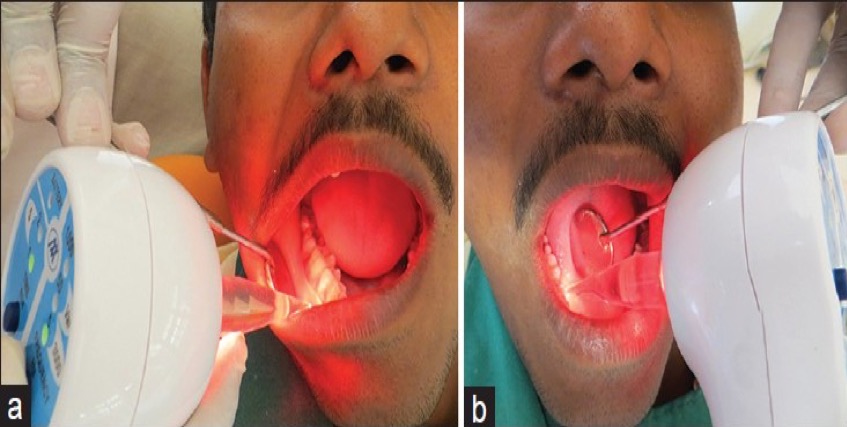 Fig 6: Low level laser therapy to treat postop pain management
Fig 6: Low level laser therapy to treat postop pain management
3) POSTOPERATIVE WOUND HEALING
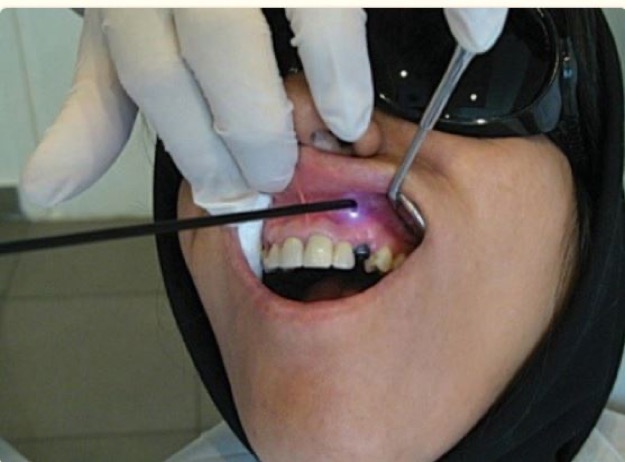 Fig 7: Low level laser therapy to accelerate post operative healing
Fig 7: Low level laser therapy to accelerate post operative healing
LLLT can be used for faster healing because of certain processes.
 4) REPAIR DAMAGED NERVE
4) REPAIR DAMAGED NERVE
Low level laser results in stimulation of damaged fibers’ axon growth.
Protocol of laser therapy includes the use of 4/5J irradiation for 10 days.
 Fig 8: Low level laser therapy to repair damaged nerve
Fig 8: Low level laser therapy to repair damaged nerve
5) ACCELERATE ANESTHESIA
In patients experiencing problems during anesthesia, with irradiation of 2 to 3 J of laser on apex of teeth, blood circulation of the area improves and anesthesia with lidocaine is obtained sooner.
 Fig 9: Laser therapy can accelerate anesthesia
Fig 9: Laser therapy can accelerate anesthesia
6) REDUCED NAUSEA DURING TREATMENT
Nausea is one of the most common problems during dental treatments. For this purpose 2 J of energy is used in the hand wrist area and P6 Meridian point.
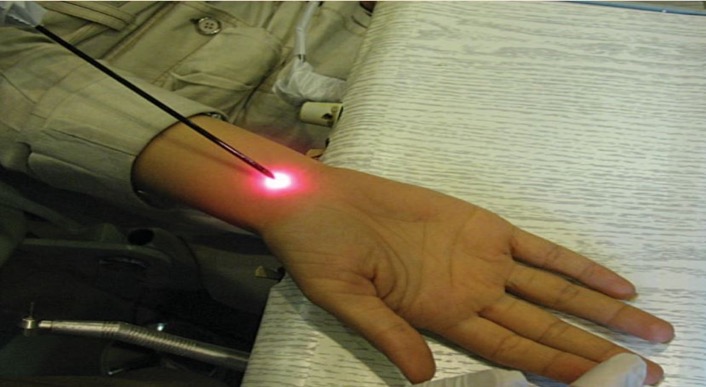 Fig 10: Laser therapy to reduce nausea during stages of root canal therapy.
Fig 10: Laser therapy to reduce nausea during stages of root canal therapy.
7) TEMPEROMANDIBULAR JOINT DISORDER
LLLT use for TMDs is beneficial because of its ease of application, analgesic, anti-inflammatory, and regenerative effects.
 Fig 11: Laser therapy to treat Tempo-mandibular joint disorders
Fig 11: Laser therapy to treat Tempo-mandibular joint disorders
8) POSTEXTRACTION HEALING THERAPY
It is useful to irradiate the area before and after an extraction.
Before extraction- Aids in faster onset of local analgesia & reduced bleeding,
After extraction– Aids in control of the swelling & inflammation.
Thus, less postoperative pain and better healing can be expected.
 Fig 12: Laser therapy to accelerate post-extraction healing
Fig 12: Laser therapy to accelerate post-extraction healing
9) ORAL MUCOSITIS
It is used as a preventive application to mucositis and as a treatment mechanism for healing erupted sores.
 Fig 13: Treatment of oral mucositis with Low level He-Ne unit
Fig 13: Treatment of oral mucositis with Low level He-Ne unit
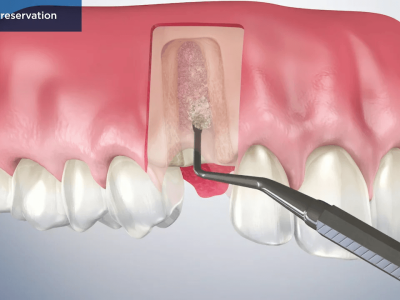
10) IMPLANT THERAPY
LLLT can effectively decrease pain sensations during the implant placement, help speed the integration of the implant into the bone and improve the quality of the bone around the implant.
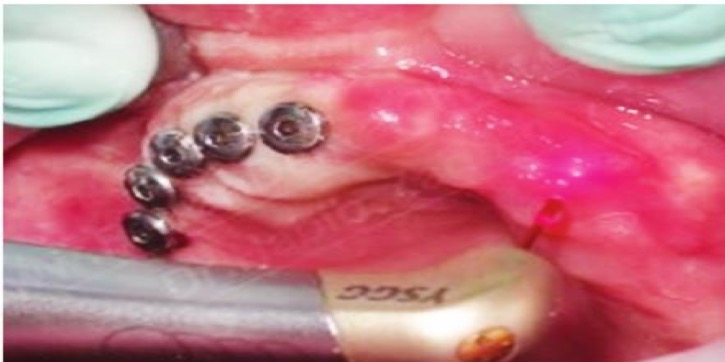 Fig 14: Application of laser during implant treatment
Fig 14: Application of laser during implant treatment
11) ORTHODONTIC THERAPY
Orthodontic treatments are lengthy and painful for many patients.
LLLT decreases the inflammation and pain caused from the pressure on the teeth during orthodontic tooth movement. LLLT stimulates osteoblasts which results in an increased velocity of tooth movement.
 Fig 15: Low level laser therapy to reduced postoperative orthodontic pain.
Fig 15: Low level laser therapy to reduced postoperative orthodontic pain.
ADVANTAGES
 DISADVANTAGES
DISADVANTAGES
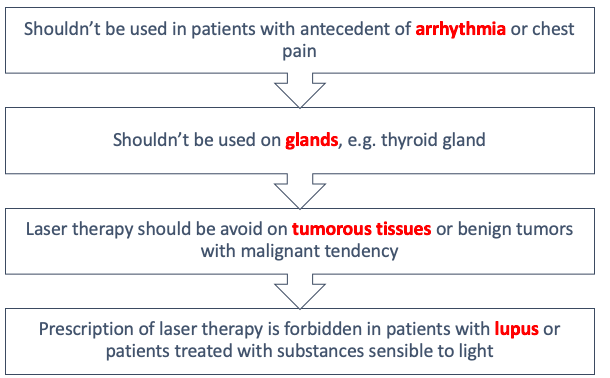
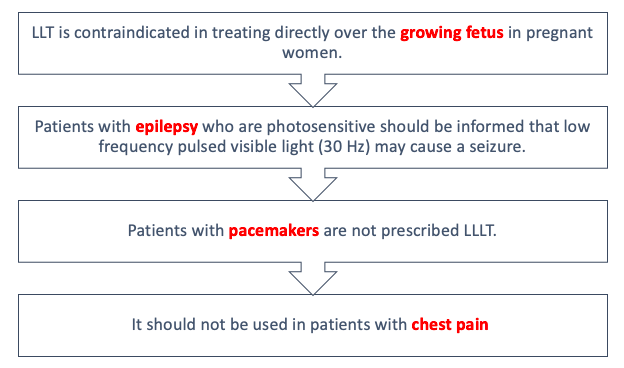
 CONTRAINDICATIONS
CONTRAINDICATIONS
 CONCLUSION
CONCLUSION
- In many dental specialties, LLLT is a useful adjunctive treatment.
- On the hard and soft tissues of the oral cavity, it has a positive effect with fewer side effects.
- In conjunction with non-surgical periodontal therapy, photobiomodulation, a process mediated by low-level lasers, promotes additional benefits in the near term, speeds up the healing of bone and gingival tissue, and lessens the side effects of periodontal surgery.
- LLLT can provide patients with a wide range of therapeutic advantages, including faster wound healing and pain alleviation.
REFERENCES
- Schwarz F, Rothamel D, Sculean A, Georg T, Scherbaum W, Becker J. Effects of an Er:YAG laser and the vector ultrasonic system on the biocompatibility of titanium implants in cultures of human osteoblast-like cells. Clin Oral Implants Res 2003: 14: 784-792.
- Kreisler M, Kohnen W, Marinello C, Gatz H, Duschner H, Jansen B, d’Hoedt B. Bactericidal effect of the Er:YAG laser on the dental implant surfaces: an in vitro study. J Periodontol 2002: 73: 1292-1298.
- Schwarz F, Jepsen S, Herten M, Sager M, Rothamel D, Becker J. Influence of different treatment approaches on non-submerged and submerged healing of ligature induced peri-implantitis lesions: an experimental study in dogs. J Clin Periodontal 2006: 33: 584-595.
- Takasaki AA, Aoki A, Mizutani K, Kikuchi S, Oda S, Ishikawa I. Er:YAG laser therapy for peri-implant infection: a histological study. Lasers Med Sci 2007: 22: 143-157
















Comments