With the advancements in adhesive dentistry, minimally invasive dentistry options are a regular at most dental practices. Why? Because it fulfils the requirements of esthetics as well as conservative dentistry. This was one of the biggest criticisms of full crowns – that they were not conservative, as we had to reduce the tooth 360 degrees, often cutting sound tooth structure to fulfil the need of mechanical strength, esthetics and function. But veneers ended up becoming a game changer, and by that I specifically mean porcelain veneers. It lasted longer than composites, had the same esthetics as a full crown did in most cases and preserved the palatal tooth structure. So, did that mean full crowns are well on their way to becoming obsolete? Au Contraire, no.
You can also read about composities vs crowns here.
Yes, minimally invasive dentistry has taken the world of dentistry by storm, so much so, that full crown cases are frowned upon for being too radical. There is now, a lot of importance being attached to Muller de Van’s dictum of tooth preservation, specifically enamel, to enhance the adhesive bonding between the veneer and the underlying tooth structure. But in the quest for esthetics and tooth preservation, somewhere along the way, functional occlusion has been forgotten.
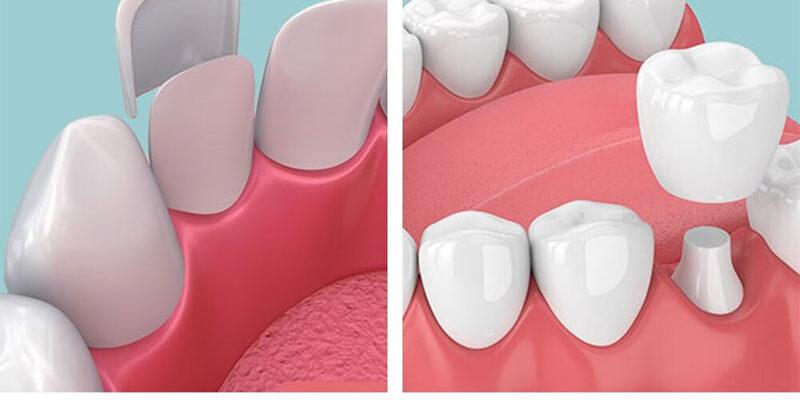
Veneers are popular because it is “additive” i.e., you can add a layer of ceramic about 0.5 – 0.8mm in thickness to the labial surface of the tooth with modifications such as an incisal / palatal wrap, with minimum tooth prep. A crown is considered “subtractive”. This means that minor proclination or alignment mismatch between anterior teeth can be corrected with the former rather than the latter.
Many clinicians enthusiastically treat a case with veneers only to find that it fractures a couple of months down the line. They don’t understand why it happened, especially when they had followed all the bonding protocols correctly, and the work had been given to a niche lab, specializing in the above.
In order to understand why the veneer fractured, we must understand its limitations, especially wrt functional occlusion. Anterior guidanceis a component of functional occlusion which is often ignored and not taken into account when doing treatment planning. According to Dawson, anterior guidance is the dynamic relationship of the lower anterior teeth against the upper anterior teeth through all the ranges of function. It plays a very important role in protecting the posterior teeth from protrusive and lateral stresses by disoccluding effect, i.e., Mutually Protective Occlusion (MPO).
Why am I stressing on “dynamic”? How is this different from static occlusion? Simply put, static occlusion refers to the position of maximum intercuspation (MIP) in dentate patients whereas dynamic occlusion refers to the entire range of movements between upper and lower teeth in function i.e., speaking, chewing and swallowing. This entire range of functional motion is referred to as “Envelope of Motion”.
So where does the Anterior Guidance fit into all of this?
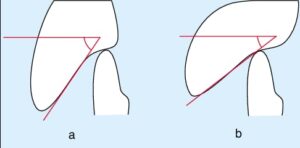
Reference – https://www.researchgate.net/figure/a-Steep-anterior-guidance-increases-likelihood-of-posterior-disclusion-b-Shallow_fig2_9052170
In the figure above, a) shows steep anterior guidance while b) shows shallow anterior guidance. Its exactly this, which determines if the case can be restored with crowns or veneers. In cases with a shallow anterior guidance, the envelope of motion / dynamic occlusion includes the anterior edge to edge position and possibly even beyond that in protrusive movements. In such cases, when veneers are given, it fractures, because the patient incises with ease due to a shallow anterior guidance. This is exactly why veneers are a double-edged sword. As they don’t involve the palatal surface of upper anteriors, the incisal guidance cannot be changed, and when the incisal edge of the veneer ends up bearing the brunt of the entire masticatory load, it ends up fracturing. These are the cases which should be managed with crowns.
Why? Is it because full crowns have better mechanical strength than veneers? No. It’s because, since full crowns involve the palatal surface of the upper anteriors, by increasing the palatal concavity, one can convert a shallow anterior guidance to a steep one. In other words, we make it very uncomfortable for the patient to include extreme protrusive movements within the scope of dynamic occlusion. By doing this, the posterior disocclusion is more in MPO and this leads to longevity of not just the anterior prosthesis, but the posterior teeth as well.
In short, by crowning the anteriors, we end up improving the functional occlusion in both the anterior as well as posterior segment. Often these results can be achieved by crowning as few as just two anterior teeth, and when compared to all the corrections in functional occlusion that can be achieved, its not that radical, a treatment option.
The other advantages of crowns include better esthetics, especially in cases where the tooth is discoloured post RCT, for that cannot be masked by a veneer. Veneers are ultra-thin and ultra-translucent glass ceramics and thus they allow light to pass through them and allow the underlying tooth structure to be reflected. This is what makes veneers so esthetic, for the tooth feels “alive”. But the same becomes a disadvantage when the non-vital tooth is already discoloured / when it starts discolouring over a period of time, especially after the veneer has already been bonded.
The other issue is, most labs do not provide clinicians with a warranty for veneers, whereas warranties for crowns are offered up to a decade and more. These two points require careful analysis and consideration and both the clinician, and the patient must be on the same page, in order to avoid any future blame – game.
As a clinician, the deciding factor between crowns and veneers, in my opinion must always be:
- functional occlusion,
- vitality of the tooth in question,
- availability or non-availability of warranty for the prosthesis and
- finally the patient’s wishes, after the first three points have been considered.
References
1.Schuyler CH. The function and importance of incisal guidance in oral rehabilitation. J Prosthet Dent 2001;86:219-32.
2.Ross IF. Incisal guidance of natural teeth in adults. J Prosthet Dent 1974;31:155-62.
3.Broderson SP. Anterior guidance: The key to successful occlusal treatment. J Prosthet Dent 1978;39:396-400.
4.Mizrahi B. The Dahl principle: Creating space and improving the biomechanical prognosis of anterior crowns. Quintessence Int 2006;37:245-251.
5.Dawson DE. Evaluation, diagnosis and treatment of occlusal problems. St. Louis: C.V. Mosby.
6.Fradeni M. Esthetic Rehabilitation in fixed prosthdontics. Vol 1. Quintessence Publishing Co,Inc.


















Comments