Introduction
Extraction socket preservation (ESP) is a critical step in modern dentistry to ensure predictable and esthetic outcomes following tooth extraction. Preservation of the tooth socket is important in the prevention of bone loss, reduction of soft tissue collapse, and maintenance of gingival architecture.

The alveolar ridge is a tooth-dependent structure that develops in conjunction with tooth eruption and undergoes volume and morphologic alteration subsequent to tooth loss. Studies have shown that unassisted natural healing of the alveolar process post extraction leads to substantial loss of the ridge volume.
Volume and morphologic alteration of alveolar ridge occur rapidly within the first 3 months to 6 months of tooth extraction and continue gradually at a slower rate thereafter[1-4] .
The term, alveolar ridge preservation, was coined due to the rationale of minimizing dimensional changes of the alveolar ridge (resorption) after tooth extraction. It involves the use of bone graft material, a membrane, and biological products either alone or in combination with one another. This is done to enhance bone formation in the socket post extraction.
When to do extraction socket preservation?
It can be done immediately after extraction or can be delayed for a period of 6-8 weeks in case of presence of acute infections.
Case selection in extraction socket preservation
Pre-operative patient assessment and treatment planning needs to be done before electing for socket preservation.
Pre-operative evaluation includes
- SYSTEMIC HEALTH STATUS
- LOCAL FACTORS
- Morphology of soft tissue & alveolar ridge volume (Lack of adequate soft-tissue coverage causes insufficient primary tension-free closure over the site of augmentation.)
- Ridge contour
- Neighbouring teeth position of marginal bone
It is imperative to scan the defect preoperatively by radiographs.
Before electing for socket preservation, one must know the classification of extraction sockets. Elian et al. proposed a simplified classification which helps to determine the bone quality following extraction based on the presence of buccal and palatal hard and soft tissues. This classification is simplified which helps the clinicians for better documentation and treatment and helps clinicians to decide if socket surgery is indicated or not whether an immediate or delayed implanted is needed or not.
- Type I socket: The facial soft tissue and buccal plate of the bone are at normal levels in relation to the cementoenamel junction of the pre-extracted tooth and remain intact post extraction
- Type II socket: Facial soft tissue is present, but the buccal plate is partially missing following extraction of the tooth
- Type III socket: The facial soft tissue and the buccal plate of the bone are both markedly reduced after tooth extraction
Type I sockets does not require any augmentation procedure and can be treated with immediate or delayed implant.
Type II and III sockets require socket treatment due to deficient buccal cortical bone and should be treated as staged approach due to socket healing additional soft and hard tissue surgery are required before implant placement[5] .

Indications of extraction socket preservation
- Decreases alveolar ridge atrophy after tooth extraction for implant prosthesis treatment
- Immediate implant placement indicated in fresh extraction sockets having one wall defect requiring adequate buccal cortical plate
- Restoration of bony defects caused by infection, trauma, and traumatic extractions
- Anterior teeth where buccal bone thickness is ≤2 mm
- Areas in close proximity to anatomic structures (maxillary sinus and mandibular canal).
Contraindications of extraction socket preservation
- Medical conditions that preclude implant placement
- Extracted socket with bony lesions of more than 5 mm where future implant cannot be placed
- It is not advisable when there is molar root‐penetrating maxillary sinus
- In cases of maxillary alveolar process atrophy and nasal floor projection which can cause risk of nasal floor perforation.
Why and where to do extraction socket preservation?

How to do extraction socket preservation?
Techniques of extraction socket preservation:
The most commonly used socket preservation techniques in dentistry include the use of bone graft materials, barrier membranes, and growth factors.
The use of autogenous bone grafts is considered the gold standard, but allografts, xenografts, and synthetic materials have been shown to have similar outcomes.
Barrier membranes are used to prevent soft tissue ingrowth and to support bone formation, while growth factors, such as platelet-rich plasma, have been shown to enhance bone regeneration.
Socket preservation technique can be categorized by the following biomaterials such as:
- Ridge preservation by only bone grafts
- Ridge preservation by membrane only
- Combined technique
- Particulate bone graft with resorbable membrane
- Particulate bone graft with platelet-rich fibrin
Grafting materials in extraction socket preservation
A. Bone Graft Materials
1. Autogenous bone
In 2005, an ESP case with autogenous bone was reported using the buccal bone of the maxillary canine and raising a rotated palatal flap. However, autogenous bone has not been widely used due to its high risk of resorption.
2. Xenogeneic bone
Currently, xenografts are generally used in implant dentistry including anorganic bovine bone and porcine bone. Artzi et al. reported 82.3% extraction socket filling with new bone at 9 months after ESP using porous bovine bone mineral (PBBM). PBBM is a biocompatible and acceptable bone substitute for ESP that shows no resorption for 9 months. In 2018, deproteinized porcine bone mineral (DPBM) exhibited comparable ESP outcomes with DBBM.
3. Synthetic bone
Several synthetic bone products have been reported to have effective outcomes on ESP, including Bioplant HTR, hydroxyapatite (HA), biphasic calcium phosphate (BCP), bioactive glass, and calcium sulfate.
4. Allogeneic bone
Allogeneic bone, such as freeze-dried bone allograft, has been widely used in implant dentistry. To improve the bone healing potential and reduce the mobility of bone graft, allogeneic bone can be manufactured as putty or gel type and can be mixed with particulate xenogeneic or synthetic bone.
5. Growth factors
Ridge preservation and bony healing can be enhanced with growth factors including recombinant human bone morpho- genetic protein-2 (rhBMP-2), platelet concentrate (platelet- rich plasma, platelet-rich fibrin), synthetic cell- binding peptide P-15 (Putty P15), and vascular endothelial growth factor (VEGF).
Socket Sealing
After packing the socket with bone substitute, it is recommended to cover it with a membrane. To perform minimally invasive surgery, flap release such as vertical releasing incisions and sub- mucosal undermining should be avoided as much as possible.
1. Autogenous tissue
Since 1997, socket sealing surgery has been used to cover the graft with free gingival tissue or connective tissue from the palate or maxillary tuberosity.
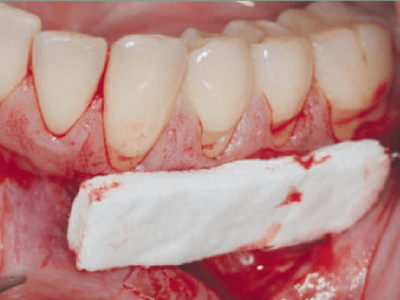
2. Acellular dermal matrix
Luczyszyn et al. introduced a technique using an acellular dermal matrix to cover the socket graft with resorbable hydroxyapatite. The hydroxyapatite affected the ESP outcome, and the matrix contributed to thickening of the soft tissue around the socket.
3. Resorbable barrier membrane
Although many researchers have demonstrated significant ESP outcomes using only a resorbable membrane to cover the socket, without bone grafting, the outcome could be maximized with bone grafting. In cases of biphasic calcium phosphate grafting with a cross-linked collagen membrane, sufficient ridge preservation occurred with prolonged barrier function even with early membrane exposure. Acceptable ESP outcomes were re- ported with polylactide and polyglycolide sponges and native bilayer collagen membranes.
4. Non-resorbable barrier membrane
Faciola Pessôa de Oliveira et al. reported successful ESP outcomes after covering with a polytetrafluoroethelene (dPTFE) membrane after minimally traumatic extraction.
5. Collagen sponge
The Bio-Col method was suggested as an effective ESP technique to pack a collagen sponge above the xenogeneic bone graft into 1/2 to 2/3rd of the extraction socket.
Complete removal of inflammatory tissue and pathologic lesions should be performed with minimally invasive procedures after tooth extraction. All soft tissues along the socket wall are removed, and spontaneous bleeding is induced to release healing factors from the bone marrow. Suturing is performed with a collagen plug, barrier membrane, or autogenous gingival tissue after application of bone substitute.
Primary wound closure is not essential if proper suturing is achieved to prevent dislodgement of the membrane or collagen plug above the substitutes.
It was said that using a osteoconductive bone substitutes such as deproteinized bovine bone material (DBBM) (Bio-Oss; Geistlich Pharma AG, Wolhusen, Switzerland) or other synthetic materials with slow resorption and covering the upper part with a resorbable barrier membrane or connective tissue graft, or selecting the BioCol procedure maintains the volume of the extraction socket well and facilitates implant placement in the future5. Implants can be placed with no complications at 4-6 months after grafting.
Controversy
1. Positive view
Since socket preservation grafting is performed to minimize ridge atrophy after tooth extraction, several advantages have been suggested, including that ESP reduces the need for additional bone graft, facilitates the implant procedure, and improves marginal bone loss and survival/success rate of implants8. Avila-Ortiz et al. reported that the ESP group had statistically significantly less bone resorption of 1.89 mm horizontally, 2.07 mm at labial side and 1.18 mm at lingual side vertically compared to the simple extraction group. In particular, the result of ESP was excellent in the maxilla. When ESP is performed in the maxillary posterior region, sinus elevation surgery can be minimized or avoided, enabling flapless implant surgery.
Natural bone healing is insufficient in extraction sockets with periodontal or inflammatory disease because soft tissue invasion into the socket impedes bone healing even long after the procedure. To maintain the volume of the extraction socket, thickness of the buccal bone wall is the most important factor. ESP is generally recommended for sockets with thin buccal bone wall (≤1 mm).
2. Negative view
Some researchers have argued a negative view of ESP. ESP can reduce the bone resorption, but not completely prevent. Rather, bone substitutes could contribute to impaired natural bone healing. Few studies reported no differences in feasibility, success/survival rates, and marginal bone loss between implants with and without ESP. Simon et al. questioned the usefulness of performing bone graft before implant placement (guided bone regeneration [GBR]+ESP) and observed that bone height loss occurred more than bone width even after bone graft. Therefore, it was argued that filling the graft material not only inside the extraction socket but also outside the extraction socket and covering it with a barrier membrane could prevent bone loss as much as possible.
Conclusion
- ESP is not required in all extraction cases, but should be considered in the following cases:
- Aesthetic concern
- Severe destruction of residual bone walls after tooth extraction
- Delayed implant treatment
2. With ESP, the necessity for additional bone grafting is reduced at implant placement.
3. ESP does not affect the success rate or marginal bone loss of implants.
4. No consensus has been made on the standard protocol among ESP techniques.
5. Socket sealing can protect bone substitutes and contribute to soft tissue healing through autogenous gingival tissues, barrier membranes, collagen sponges, etc.
6. During ESP, primary closure is not essential, but minimally traumatic procedures are very important.
7. Dental implants are recommended to be placed 4 months after ESP.
Based on current evidence, extraction socket preservation/augmentation is suggested not only in clinical cases with dental implants being planned but also to preserve alveolar bone for removable prosthesis fixation or to support soft tissue around fixed dental prosthesis. Further studies are needed to validate the reliability of proposed clinical decision tree for extraction socket augmentation.
References
1. Schroeder HE. The periodontium. Berlin: Springer-Verlag; 1986.
2. Atwood DA, Coy WA. Clinical, cephalometric, and densitometric study of reduc- tion of residual ridges. J Prosthet Dent 1971;26:280–95.
3. Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 2003;23:313–23.
4. Tan WL, Wong TL, Wong MC, et al. A systematic review of post-extractional alve- olar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 2012;23(Suppl 5):1–21.
5. Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007 Mar;19(2):99-104; quiz 106. PMID: 17491484.
6. Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent 2007;19:99‐104.
7. Haggerty C, Laughlin R. Extraction Site (Socket) Preservation. Atlas of Operative Oral and Maxillofacial Surgery. John Wiley & Sons, Inc.; 2015.
8. Kim, Young-Kyun & Ku, Jeong-Kui. (2020). Extraction socket preservation. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 46. 435-439. 10.5125/jkaoms.2020.46.6.435.
9. Juodzbalys G, Stumbras A, Goyushov S, Duruel O, Tözüm TF. Morphological Classification of Extraction Sockets and Clinical Decision Tree for Socket Preservation/Augmentation after Tooth Extraction: a Systematic Review. J Oral Maxillofac Res. 2019 Sep 5;10(3):e3. doi: 10.5037/jomr.2019.10303. PMID: 31620265; PMCID: PMC6788426.
















Comments